Multidisciplinary approach key to optimizing outcomes

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/df8c486a-747e-4777-8c63-f83bf4561c61/20-WHI-2027280_CQD_650x450_jpg)
20-WHI-2027280_CQD_650x450
Up to 1% of women with pelvic endometriosis have endometriosis involving the urinary tract. In cases of deep endometriosis (DE), the prevalence is even higher — up to 50%. Yet even in the latter cases when symptoms are obvious, urinary tract endometriosis (UTE) remains underdiagnosed, according to Rosanne M. Kho, MD, Head of the Section of Medical Gynecology and Minimally Invasive Gynecologic Surgery at Cleveland Clinic’s Ob/Gyn & Women’s Health Institute. She is one of several experts from around the world who recently co-authored a comprehensive review on the topic in Diagnostics.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Diagnosing UTE can be challenging; unless clinicians have a high index of suspicion, it’s often missed,” says Dr. Kho. “The more we can do to educate them and raise awareness the better, because patients often have pain and symptoms from this disease for years before getting the correct treatment.”
Of women with UTE, 85% have disease in the bladder, 10% in the ureter, 4% in the kidney, and 2% in the urethra. One reason that the differential diagnosis is complicated is that the presentation of bladder DE can vary and the symptoms may mimic other urinary tract issues. Symptoms are absent in about half of women with ureteral disease, whereas 25% have flank pain and 15% gross hematuria.
“Many patients with UTE are asymptomatic until the disease is severe. But in women with DE, it can present as cyclic hematuria, urinary urgency or urinary frequency,” Dr. Kho says. “Urinary tract infections also can be one of the presentations. Urinary incontinence and retention are rare.”
The etiology of UTE is unclear but the pathogenesis may be related to retrograde menstruation, coelomic metaplasia, spread of endometrium-derived stem/progenitor cells, and altered genetic/epigenetic or immune factors. Some evidence suggests that bladder endometriosis is more common in women who have had a cesarean section.
Endometriosis at other anatomic sites is common in women with UTE, making medical history and physical examination important for diagnosis. Urinalysis should be performed when dysuria, urinary frequency or hematuria are present, and culture if infection is suspected. For ureteral DE, tissue biopsy and histology are the gold standard.
Advertisement
In terms of imaging, ultrasound is the method of choice for UTE. A transvaginal approach is appropriate for bladder DE and a transabdominal for the assessment of suspected ureteral disease. The latter also should be used in cases of ureteral DE to rule out hydronephrosis, which is often asymptomatic.
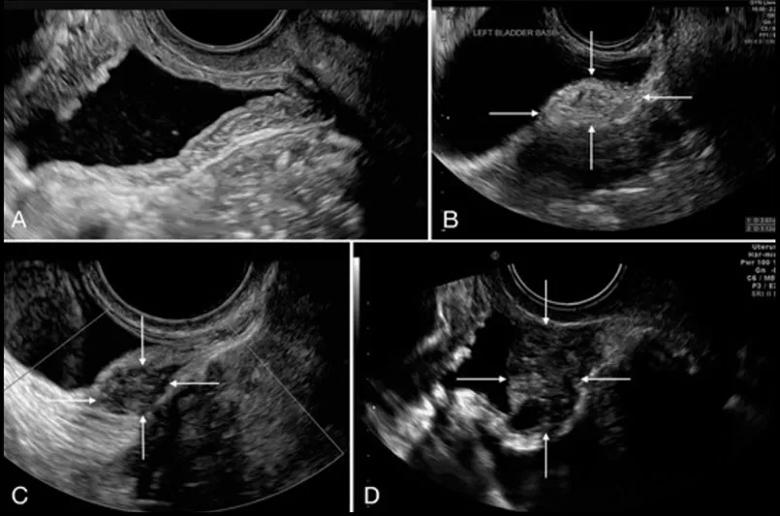
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4904936c-0cfb-4012-a0a1-9293ab26baa2/20-WHI-2027280_CQD_inset_805x533_2_jpg)
Transvaginal ultrasound depiction of the bladder. (A) Normal bladder and (B–D) three bladder deep endometriosis nodules, identified with white arrows.
Magnetic resonance imaging (MRI) can be considered as an alternative to transvaginal ultrasound or for presurgical staging of UTE.
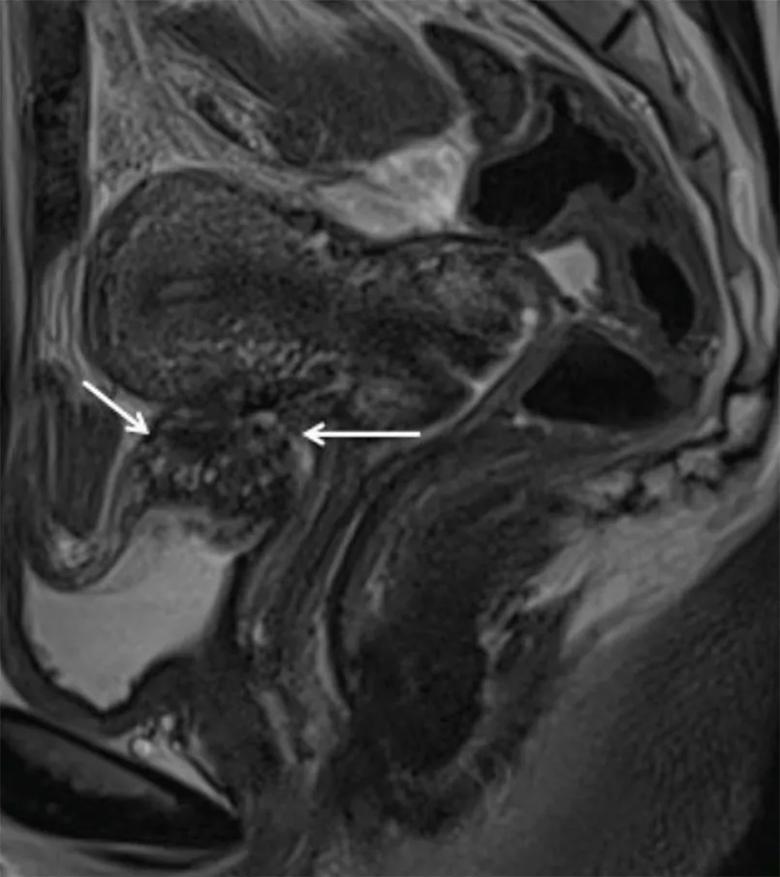
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0cee8b41-8343-4241-ba65-48c57ba0568a/20-WHI-2027280_CQD_inset_805x905_5_jpg)
Magnetic resonance imaging depiction of bladder deep endometriosis. Sagittal T2-weighted plane depicting deep endometriosis nodule in hyposignalT2, which is infiltrating the detrusor muscle of the bladder (white thin arrows).
In terms of treatment, the approach varies depending on symptoms and the presence of ureteral obstruction or hydronephrosis. Surgery is usually necessary for ureteral DE, whereas both medical and surgical options exist for bladder DE.
“When it comes to DE, the great majority of the time, surgical treatment is preferable for definitive treatment,” says Dr. Kho. “Surgery for bladder DE often involves extensive dissection. These are advanced procedures — the risk of complications is high and the recovery can be prolonged.”
“For patients with comorbidities who are not surgical candidates, we will try a medical approach,” Dr. Kho continues. “Our hope is that they will respond and we can get them through to menopause, when the disease tends to recede.”
Advertisement
Medical approaches for pain associated with bladder DE include continuous progesterone-based regimens administered orally or via an intrauterine device, implant or injection; combined estrogen-progesterone therapy; or gonadotropin-release hormone (GnRH) analogues. Surgery, which is usually done laparoscopically or robotically, consists of shaving serosal lesions and full-thickness resection of DE lesions.
Given the complexity of diagnosis and management of UTE, Cleveland Clinic has implemented a team-based approach to the disease.
“We have implemented a comprehensive imaging protocol with our colleagues in Radiology, which enables the diagnosis of endometriosis preoperatively. This facilitates a multidisciplinary approach and plan for surgical treatment. It also allows for shared decision making with the patient. If surgical intervention is necessary, we collaborate with colorectal surgery, urology, vascular surgery and cardiothoracic surgery. Our multidisciplinary Center for Endometriosis and Chronic Pelvic Pain also includes medical pain specialists, pain psychologists, and physical and occupational therapists. Together, we work with patients to optimize outcomes and recovery,” Dr. Kho concludes.
*Note: Images originally published in: Leonardi, M.; Espada, M.; Kho, R.M.; Magrina, J.F.; Millischer, A.-E.; Savelli, L.; Condous, G. Endometriosis and the Urinary Tract: From Diagnosis to Surgical Treatment. Diagnostics. 2020;10:771.
Advertisement
Advertisement
Increasing uptake remains a challenge
Multidisciplinary teams work together in in-situ scenarios
Uterine transposition cleared the field for radiation therapy
ACOG-informed guidance considers mothers and babies
Prolapse surgery need not automatically mean hysterectomy
Artesunate ointment shows promise as a non-surgical alternative
New guidelines update recommendations
Two blood tests improve risk in assessment after ovarian ultrasound