Therapies include steroid implants, immunomodulation and biologics
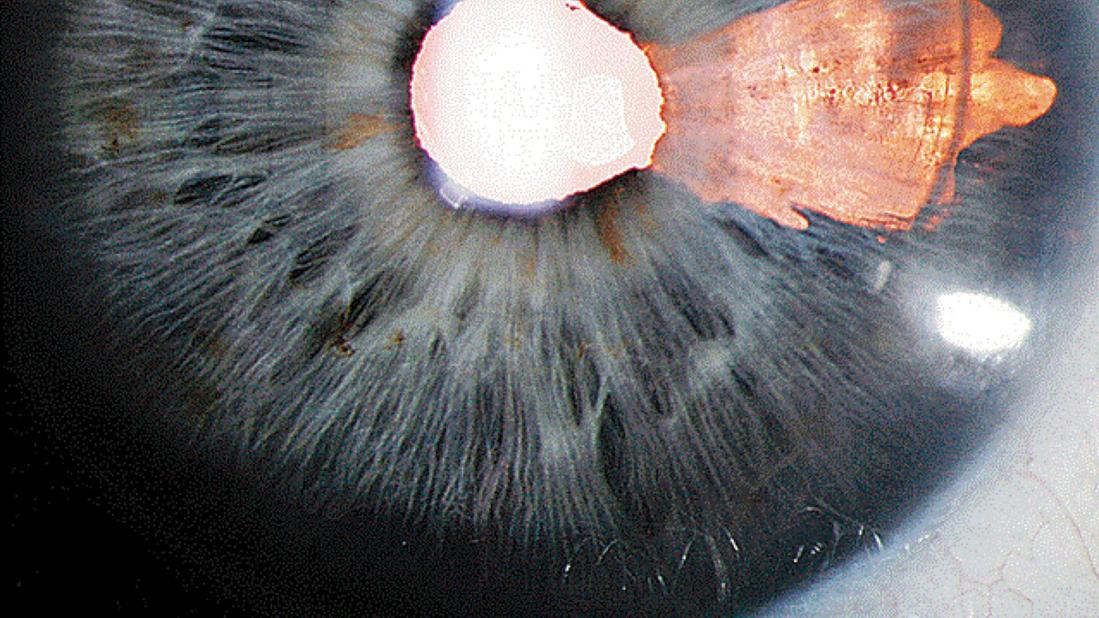
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/89b5d9ae-d544-4cb4-81b7-860293edbc43/viral-infection-uveitis)
Uveitis caused by a viral infection
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a referral practice like the one at Cleveland Clinic Cole Eye Institute, a small percentage of patients with uveitis have infectious uveitis, a larger percentage have known etiologies of noninfectious uveitis like sarcoid or birdshot, but more than 50% have idiopathic or undifferentiated uveitis. We need better diagnostics to classify this disease so we can treat it most effectively.
The most common types of infectious uveitis that we see in clinic are caused by herpes viruses (e.g., herpes simplex virus, varicella-zoster virus, cytomegalovirus) and toxoplasmosis. Unfortunately, we usually have to empirically treat these patients based on clinical findings alone, because getting results of polymerase chain reaction (PCR) testing from an outside lab takes about one week.
Two labs have investigated different types of rapid multiplex PCR testing. One team used real-time PCR with melting curve analysis, looking at the infectious organisms most commonly seen in uveitis. In less than two hours, they were able to get results at very high sensitivity and specificity compared to singleplex PCR testing for these organisms.
Another team published a case report in which they took a swab from a corneal ulcer and analyzed it with a commercially available panel of nested multiplex PCR followed by a melting curve analysis developed for meningoencephalitis as well as septicemia blood culture identification. In under 1.5 hours, they were able to determine that the patient had a Pseudomonas corneal ulcer. However, this commercially available test has not been validated for uveitis or keratitis.
Advertisement
Then there’s metagenomic deep sequencing. This is unbiased deep sequencing. One research team developed a unique method to detect RNA and DNA viruses as well as parasites and fungi — anything that could potentially cause uveitis. In one patient with chronic bilateral uveitis and immunosuppression, the team was able to diagnose rubella. While the method is investigational and not rapid, we can see how important it is to be able to identify novel pathogenic etiologies for uveitis.
Another study evaluated the ability to use single-cell RNA sequencing to see patterns of molecular identification of uveitis. The team studied four patients with granulomatous uveitis and found several overlaps in B- and T-cell clonotypes, as well as some unique features in these patients. Although this was a very small study, a much larger longitudinal study using these techniques would potentially help us better classify uveitis and then be able to determine treatment response.
There are newer ways of thinking about how we treat uveitis, from local steroid injections to systemic steroid-sparing immunomodulation, as well as local and systemic biologics. But there are still indications for tried-and-true treatments, such as the fluocinolone acetonide intravitreal implant (0.59 mg; releases 0.3-0.4 μg of fluocinolone acetonide per day for 30 months). This treatment may be indicated for:
Advertisement
The seven-year MUST study showed faster and more complete control of inflammation with the steroid implant versus systemic therapy. But by seven years, when the implant had expired, systemic immunosuppression did a little better in terms of visual acuity (7.2 letters). The implant has its benefits, but it comes with increased risk for glaucoma surgery (45% implant vs. 12% systemic therapy) and cataract surgery (90% implant vs. 50% systemic therapy).
The dexamethasone intravitreal implant for noninfectious uveitis lasts only about three to four months. It also comes with expected rates of glaucoma (7.1% implant vs. 4.2% sham) and cataract (15% implant vs. 12% sham), according to the Ozurdex HURON study group.
The POINT trial showed us how to compare periocular steroids versus intravitreal steroids. We have to remember that:
Then the fluocinolone acetonide insert was developed and also was effective at decreasing recurrence of noninfectious uveitis. The rate of cataract remained higher in patients with the insert versus sham (33% vs. 12%). The rate of glaucoma was equivalent (26% insert vs. 26% sham).
Suprachoroidal steroid injections (CLS-TA) were approved by the U.S. Food and Drug Administration in 2021 for the treatment of uveitic macular edema. The rates of glaucoma (11.5% CLS-TA vs. 15.6% sham) and cataract (7.3% CLS-TA vs. 6.3% sham) were not terribly high.
Advertisement
When treating noninfectious uveitis today, we start with systemic steroid-sparing immunomodulatory therapy (e.g., methotrexate, mycophenolate, azathioprine) as first line. Second-line agents are usually the tumor necrosis factor-alpha (TNF-alpha) inhibitors (e.g., adalimumab, infliximab). Then third-line agents are biologics that target other inflammatory cytokines, like interleukin 6 (IL-6) or B cells.
It takes time to go down this treatment ladder, so we often bridge therapies with steroids. Ultimately, patients can be put on a lot of steroids. That’s when we need to consider local steroids instead of systemic steroids. If using a third-line immunomodulatory agent, perhaps a long-acting local steroid would be best. Today we are much more intentional about using local steroids with systemic immunomodulation in uveitis patients.
Tried-and-true but off-label use of some of the first-line agents above was studied in the FAST trial. The study compared oral mycophenolate with oral methotrexate in patients with uveitis and found that both treatments were effective. The study did not evaluate subcutaneous methotrexate, however, which has better bioavailability.
Biologics mostly target inflammatory cytokines. The most common biologics for noninfectious uveitis are TNF-alpha inhibitors adalimumab and infliximab. Adalimumab was studied in VISUAL I, II and III trials and found to be very effective. It also was studied with methotrexate in juvenile idiopathic arthritis-associated uveitis in the SYCAMORE trial and found to be very effective. Now it has become our regular armamentarium for pediatric patients with uveitis.
Advertisement
There is some evidence that TNF-alpha inhibitor certolizumab may be effective in patients with uveitis not controlled by other TNF-alpha inhibitors. Certolizumab was evaluated in a phase 4 study of uveitis associated with axial spondyloarthropathy.
One emerging therapy that targets TNF-alpha is licaminlimab, which is an antibody fragment that targets TNF-alpha more potently than full-length antibodies adalimumab and infliximab. Because of its small molecular weight, it penetrates the ocular surface better and, thus, potentially can be effective for treatment via eye drop. It’s currently being investigated in a phase 2 trial for dry eye disease as well as being studied for uveitis.
IL-6 is a pleiotropic cytokine that’s produced by many cell types and has effects such as promoting differentiation of Th17 cells. Tocilizumab is one drug that targets the IL-6 receptor. The STOP-Uveitis trial showed it to be effective, especially for uveitic macular edema. In a retrospective study by the French Uveitis Network, tocilizumab was found to more effectively control uveitic macular edema than did TNF-alpha inhibitors — although it didn’t show a difference in steroid sparing or relapse rate.
Vamikibart is an emerging therapy targeting IL-6 that is designed for intravitreal use and fast systemic clearance. The half-life after intravitreal dosing is approximately seven days, similar to faricimab. It binds to the IL-6 receptor and prevents both cis- and trans-signaling. A phase 1 trial showed that patients with uveitic macular edema who received any dose of vamikibart had improvement in best-corrected visual acuity and central subfield thickness. The drug was well tolerated. It has been fast-tracked for phase 3 studies, which are ongoing.
Downstream from the cytokine receptors are Janus kinase (JAK) and signal transducer and activator of transcription (STAT) proteins. JAK-STAT inhibitors are advantageous because they can be developed as small-molecule inhibitors and taken orally. JAK-STAT inhibitors include:
An emerging therapy is the dual TYK2/JAK-1 inhibitor brepocitinib, which could have a broader effect because it targets more cytokine pathways. It is being studied in a phase 2 trial for treating active noninfectious uveitis.
In summary, there is a need for more rapid and specific detection of infectious uveitis, which may involve molecular classification. Short- and long-acting steroid implants are useful in treating noninfectious uveitis and are increasingly used to spare systemic steroids or bridge efficacy of immunomodulatory therapy. There are many options for steroid-sparing therapy (e.g., biologics, immunomodulatory therapy), but additional local and systemic biologic development is needed.
Dr. Lin is a vitreoretinal and uveitis specialist at Cleveland Clinic Cole Eye Institute. This article was based on Dr. Lin’s presentation at the 2024 Cole Eye Institute Retina Summit.
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Registry data highlight visual gains in patients with legal blindness
A look at emerging technology shaping retina surgery
Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs
The advanced stage of diabetic retinopathy is among the most challenging for retinal surgeons
A multitude of subspecialities offer versatility, variety
It’s the first step toward reliable screening with your smartphone