New studies shed light on infection risk factors, role of hematomas
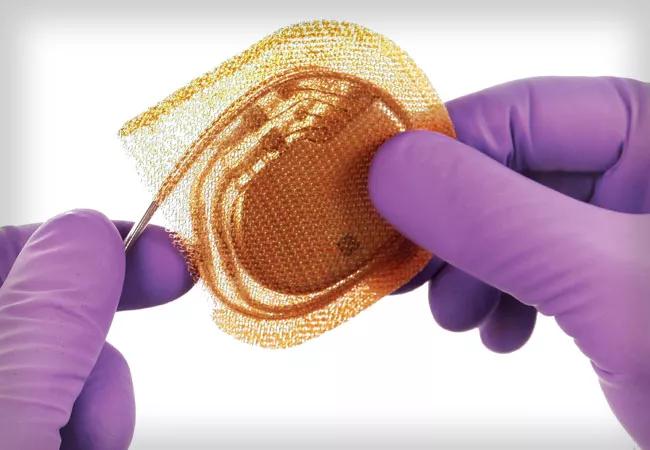
Results of the landmark Worldwide Randomized Antibiotic Envelope Infection Prevention Trial (WRAP-IT), published in 2019 in the New England Journal of Medicine, showed that placing cardiac implantable electronic devices (CIEDs) inside an absorbable, antibiotic-eluting envelope reduced the incidence of major infection by 40% within 12 months after CIED replacement, upgrade or revision or after de novo implantation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Prior to WRAP-IT, the only infection-prevention intervention with good supporting data was perioperative systemic antibiotic use,” says WRAP-IT global principal investigator Khaldoun Tarakji, MD, MPH, Associate Section Head of Cardiac Electrophysiology at Cleveland Clinic. “WRAP-IT identified the additional value of the antibiotic envelope as a second intervention to reduce infection, especially among high-risk patients.”
Since then, multiple substudies of WRAP-IT have delved deeper into various aspects of CIED infection and prevention, as well as the effectiveness and cost-effectiveness of the TYRX™ absorbable antibiotic envelope. Two of the most recent substudies are profiled here:
Although a variety of risk factors for CIED infection had been previously identified, many were nonmodifiable, leaving little opportunity for changing practices or techniques. Modifiable risk factors related to secondary procedures (i.e., device replacement or upgrade) have remained largely unknown or have lacked solid supportive evidence.
As a randomized trial with 6,800 patients treated by 700 implanters in 25 countries using local approaches, WRAP-IT provided a unique opportunity to fill these knowledge gaps. But the risk of device infection was so small, and the number of variables so large, that traditional statistical analyses were challenging. Overcoming this problem required a new approach.
Advertisement
“We employed a novel multivariate machine-learning model to identify which variables were important during secondary procedures,” says Dr. Tarakji, who served as lead and corresponding author of this analysis.
Ultimately, eight potentially modifiable procedure-related variables were found to increase the risk of infection:
Conversely, several procedure-related factors were associated with decreased risk of infection:
“Some of the findings echoed previous knowledge, but others could potentially change practice,” Dr. Tarakji says, such as whether or not to do a capsulectomy, whether to use vancomycin or cephalosporin as the perioperative antibiotic of choice and whether to use chlorhexidine or iodine for skin preparation.
The other new WRAP-IT substudy focused on the incidence of hematoma within 30 days after a secondary CIED procedure or de novo biventricular defibrillator implant, along with associated infections. It showed that within the WRAP-IT control group (i.e., patients who did not receive the antibiotic envelope), those with hematoma were far more likely than those without hematoma to develop a major infection (13.1% vs. 1.6%; hazard ratio [HR] = 11.3 [95% CI, 5.5-23.2]: P < 0.001). “This represents an 11-fold increase in the risk of infection,” Dr. Tarakji notes.
Advertisement
The analysis revealed that the incidence of hematoma in WRAP-IT was 2.2% overall and similar between patients who received the envelope and controls who did not. However, among patients who developed hematoma, the risk of a major infection over 36-month follow-up was significantly lower in the envelope group than in the control group (2.5% vs. 13.1%; HR = 0.18 [95% CI, 0.04-0.85]; P = 0.03).
“Hematoma is not rare, and both smaller and larger hematomas substantially increase infection risk,” says WRAP-IT steering committee chair Bruce Wilkoff, MD, Director of Cardiac Pacing and Tachyarrhythmia Devices at Cleveland Clinic. “This analysis shows that this infection risk was significantly mitigated with use of the absorbable antibiotic envelope.”
Dr. Wilkoff notes that the risk of hematoma increases with use of anticoagulants and antiplatelet medications. “These medications are very common in device patients and, when combined, multiply the risk of hematoma development,” he says. “Managing infection risk through hematoma prevention and use of the envelope seems to be the most effective strategy.”
The cost-effectiveness of the envelope depends on the incidence of infection, the researchers note. Although the 12-month infection rate in the WRAP-IT control group was 1.2%, the global infection rate in the general population is 2% or higher. “With an infection rate that high, the cost-effectiveness of the envelope is compelling,” says Dr. Wilkoff (see the WRAP-IT cost-effectiveness analysis in Circulation: Arrhythmia and Electrophysiology [2020;13(10):e008503]).
Advertisement
“We need to avoid the formation of hematomas through meticulous hemostasis and proper management of blood thinners,” says Dr. Tarakji, adding that this is the subject of the next WRAP-IT substudy.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more