Two-day procedure prevents neurologic compromise for octogenarian

An 82-year-old woman presented to Cleveland Clinic with right shoulder pain. An MRI of the spine revealed an incidental left paravertebral mass measuring 4.2 cm in maximal direction. There was extension into the T3 intervertebral foramen with remodeling of the adjacent vertebrae.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Because of the relative lack of symptoms on the left and the patient’s concern about having a major surgery at her age, she consulted with the spine team and decided on observation,” says Daniel Raymond, MD, a thoracic surgeon in the Miller Family Heart, Vascular & Thoracic Institute at Cleveland Clinic.
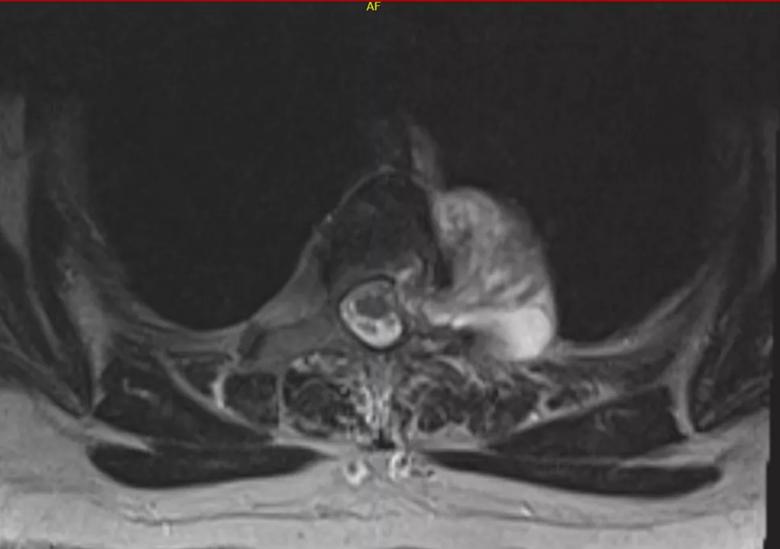
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3e930b61-005a-46bc-8671-a67658560a42/Schwannoma-1024x721_png)
A mass can be seen pushing the patient’s spinal cord to the right. The tumor extends through the neuroforamen from the outside and into the spinal canal.
During the surveillance period, the patient began to develop pain over her left scapula. She underwent physical therapy, but the pain continued intermittently. Seventeen months after her initial MRI, repeat imaging showed significant extension of the schwannoma into the spinal canal, with compression of the thecal sac and contact with the spinal cord.
“Typically, you wouldn’t expect to see a dramatic change in a schwannoma in only a year or so,” says Dr. Raymond. “In this case, the tumor was pushing on the patient’s spine, causing symptoms and growing relatively quickly.” He and Richard Schlenk, MD, a neurosurgeon and Neurosurgery Residency Training Program Director at Cleveland Clinic, decided that a hybrid resection of the dumbbell-shaped schwannoma was the best course of action.
Dr. Schlenk performed a T2-3 laminectomy using a standard posterior approach to the spinal component of the paravertebral mass. The following day, Dr. Raymond performed robotic thoracic surgery on the remaining intrathoracic component, encircling and removing the mass located on top of the aorta.
Advertisement
The surgeons opted for a two-day procedure due to the patient’s age and her concerns about the recovery process.
“The stress on the system can be a lot for an octogenarian, so we do the spine surgery first and allow the patient to recover overnight,” explains Dr. Raymond. “This approach gives us an opportunity to medically optimize our patients before putting them through a second significant operation.”
The patient in this case had an uncomplicated postoperative course and was discharged home on day four. Pathology results confirmed a grade 1 spinal schwannoma. Her long-term prognosis is excellent.
Dr. Raymond credits the success of the surgery to collaboration among the multidisciplinary team. “We have a great system. It’s not about the individual surgeon: It’s the team and culture,” he says.
Working in tandem, clinicians from thoracic surgery and neurosurgery charted a course to treat the patient based on her physiological status, not her chronological age.
“So often, we see people in our clinic who have been told they are too old for surgery,” says Dr. Raymond. “A person like this patient is clearly a candidate for surgery. We gave her an excellent operation and prevented her from serious neurologic compromise. She did great.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient