Study finds high levels of a CD8 T-cell subpopulation to be predictive of ICI resistance
Using a transcriptomic profile of a unique subpopulation of CD8 T cells from melanoma patients, a group of Cleveland Clinic investigators has developed a predictive model of immune checkpoint inhibitor (ICI) therapy response. The model is capable of distinguishing responders from non-responders with 88% accuracy by analyzing either tumor or peripheral blood CD8 T cells.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, published in the Journal of Experimental Medicine, represents a major advance in the management of patients with melanoma.
“This model may become a focused tool to help clinicians predict who and who will not respond to standard-of-care immunotherapies,” explains Brian Gastman, MD, lead investigator and Director of Cleveland Clinic’s Melanoma & High-Risk Skin Cancer Program. “This allows us to pivot treatment to the growing myriad of options being introduced to the field. Further studies will reveal whether this model can be used dynamically to reflect the changes in patients as they may develop acquired resistance, increasing its utility.”
The management of metastatic melanoma has changed in recent years, with targeted therapy and immunotherapy completely replacing chemotherapy. Very recent studies now point to the advantage of first-line immunotherapy over targeted therapy for the treatment of advanced disease, Dr. Gastman explains.
“About 45% of our patients are candidates for targeted therapy, but the data clearly shows that immunotherapy is a much more effective way of curing patients when you put the two treatment strategies head to head,” he says. “You’ve got one really good shot with immunotherapy, but if a patient doesn’t respond, you’ve got to figure out what else to do with them.”
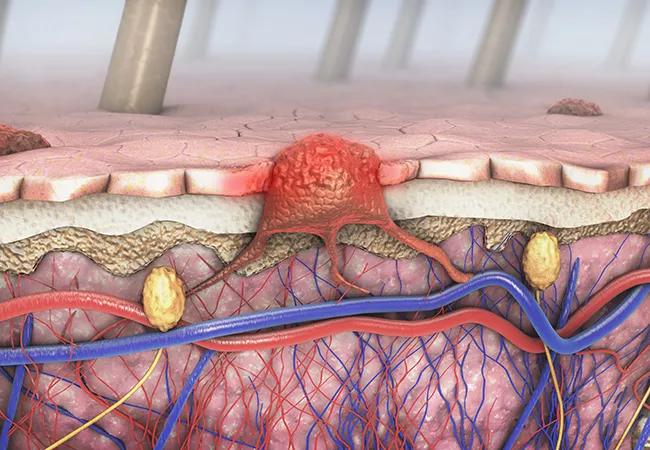
Approximately 40% of patients with melanoma will fail to respond to immunotherapy, and the lack of a predictive model of ICI response remains a significant unmet need in this population. Aside from PD-L1 expression, which is used to predict immunotherapy response in lung cancer, smaller studies have analyzed the levels of tumor-infiltrating lymphocytes (TILs) and other blood markers as potential predictors of response. However, none of these attempts have been clinically validated.
Advertisement
“Other than doing imaging, performing a physical exam, and clinically monitoring the patient, there is no effective companion tool to tell us who will or will not do well,” he says.
Prior studies have shown that TILs, including CD8 T cells, express high levels of ICI receptors, such as PD-1. It has also been established that CD8 T cell tumor infiltration correlates highly with anti-PD-1/PD-L1 immunotherapy response across different cancer types.
Based on earlier comparative studies, Dr. Gastman and his collaborators hypothesized that unique subpopulations of CD8 T cells exist in both the tumor and peripheral blood of patients with melanoma. Therefore, in this latest study, they performed a detailed characterization of CD8 T cells from the tumors and peripheral blood of eight patients with advanced melanoma and employed single-cell transcriptomic analysis to cluster different cell types.
Indeed, the cluster analysis revealed a unique subpopulation of CD8 T cells with high levels of oxidative phosphorylation in peripheral blood and tumor tissue. The authors identified this population as CD8+ TOXPHOS cells.
“We were able to figure out that these CD8 T cells not only exist in the tumor, but that they also exist at a higher level in the blood of patients who were immunotherapy resistant,” Dr. Gastman explains. “We then validated that finding against a number of patient blood samples.”
Following, the team developed a predictive model of ICI therapy response using a transcriptomic profile of CD8+ TOXPHOS cells. The model successfully predicted the ICI response in 11 of 12 patients from the training data set, resulting in a 92% predictive accuracy. It was validated further using three additional data sets, with an overall predictive accuracy of 88%. Interestingly, the model demonstrated 100% accuracy in a small cohort of lung cancer patients.
Advertisement
According to Dr. Gastman, the implications of these findings could be vast — not only in predicting ICI resistance, but also in the potential therapeutic targeting of CD8+ TOXPHOS cells.
“We discovered multiple potential targetable pathways that are relatively unique to these cells, so we want to leverage their uniqueness to go right after them therapeutically,” he says. “If we can understand the mechanisms that make these cells tick, we can go directly after them to change the course of immunotherapy.”
He notes that several important questions remain to be answered on this path of discovery, including whether these cells cause resistance without any therapy, get generated after ICI treatment, or are part of the resistance mechanism after a patient loses their response.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors