Preoperative chemotherapy enables successful surgical resection
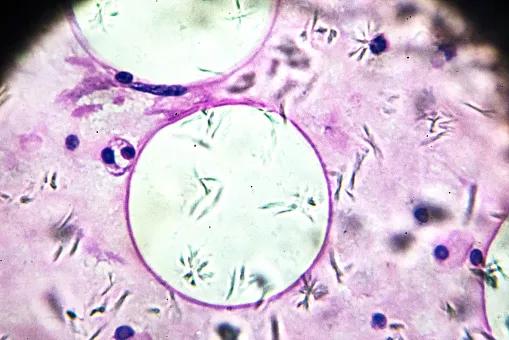
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0f444bae-f576-4d68-a3a7-d1e79c20e8b8/Thoracic-Inlet-Mass_jpg)
Liposarcoma biopsy under microscopy zoom in different ranges
A 45-year-old woman from Illinois had an enlarging thoracic inlet mass that had been initially identified in 2018 by a local physician and was assumed to be benign. Due to tumor growth, the patient underwent a needle biopsy in Chicago three years later, which revealed a low-grade mesenchymal process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In early 2021, the patient had a virtual consultation with Daniel Raymond, MD, a thoracic surgeon in the Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute at Cleveland Clinic, for a second opinion. Her only symptom was mild difficulty swallowing; however, given the size and location of the tumor, Dr. Raymond recommended a second biopsy.
The patient had an ultrasound-guided core needle biopsy in Cleveland Clinic’s Head & Neck Institute in mid-February 2021, which revealed a 7 x 7 x 10 cm myxoid liposarcoma nestled between the esophagus, trachea and aortic arch.
“Because of their rarity, sarcomas are frequently misdiagnosed on biopsy,” says Dr. Raymond. “Most pathologists aren’t experienced in diagnosing sarcomas, so it’s paramount that such cases be evaluated by an expert in soft tissue tumors.” Cleveland Clinic’s soft tissue pathology group is led by Brian Rubin, MD, PhD, Chair of the Robert J. Tomsich Pathology & Laboratory Medicine Institute and an expert in the diagnosis of sarcoma.
Based on the biopsy results, the patient underwent a multidisciplinary evaluation at Cleveland Clinic.
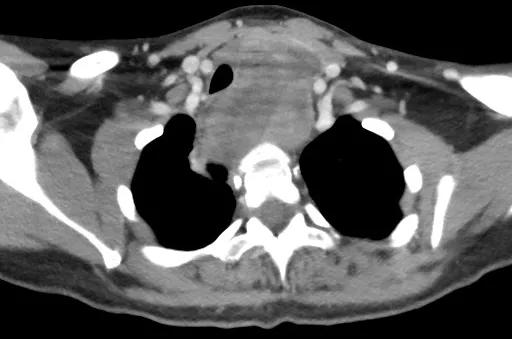
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/19ff8ced-d443-4030-8e7d-d54b3839c444/Raymond-A_png)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0c04476b-858c-446f-88d8-284cb8481631/Raymond-B_-2_png)
The patient’s initial evaluation revealed a myxoid liposarcoma nestled between the esophagus, trachea and aortic arch.
The case was reviewed by Cleveland Clinic’s sarcoma tumor board, and the team embarked on a treatment plan that included induction chemotherapy and radiation therapy followed by surgical resection.
The patient underwent two cycles of ifosfamide concurrent with a radiation dose of 46 Gy in 23 fractions at her home healthcare facility in Chicago. Afterward, she returned to Cleveland Clinic for surgical resection. Preoperative imaging revealed a significant reduction in the mediastinal mass.
Advertisement
“The patient had a remarkable response to the induction therapy,” says Dr. Raymond. “Her mass decreased to 3 x 2 x 9 cm, which gave us the opportunity to perform a more reasonable oncologic resection.”
The patient’s tumor was located predominantly in her neck, so a team led by Dr. Raymond and Eric Lamarre, MD, a surgeon in the Head & Neck Institute, performed a collar incision and midline sternotomy. Cardiac and vascular surgeons were available to assist, if necessary.
“We had to skeletonize the patient’s thoracic inlet structures, including the trachea, esophagus, innominate veins and great vessels,” explains Dr. Raymond. “Fortunately, we were able to do so without the need for major vascular resection and reconstruction.” The team was also able to preserve the recurrent laryngeal nerve in the tracheoesophageal groove, thereby circumventing any impairment to the patient’s voice.
The patient had an uncomplicated postoperative course and was discharged on postoperative day 3. She completed four cycles of adjuvant chemotherapy and shows no evidence of recurrent disease.
Dr. Raymond attributes this success to the team’s interdisciplinary collaboration and the patient’s response to preoperative induction chemotherapy.
“We have the advantage of being able to assemble a group of highly skilled clinicians in one room – oncologists, radiologists, pathologists and surgeons,” he says. “We’re able to solve difficult problems by sharing our expertise.”
Dr. Raymond notes two important points from this case. First, sarcomas are frequently misdiagnosed. Therefore, it’s important to confer with expert pathologists who specialize in soft tissue tumors. Second, there are surgical options for resecting tumors in difficult locations. The patient in this case was told she wasn’t a candidate for tumor resection surgery prior to consulting with Dr. Raymond.
Advertisement
“We frequently see patients who have been told they are not candidates for surgery because their tumors involve different structures or cross barriers – from the abdomen into the chest or the neck into the chest,” explains Dr. Raymond. “These kinds of procedures may initially be too daunting for many surgeons – but, by working together, there are few limits to what our multidisciplinary teams can accomplish.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches