Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

A new focus on cardiovascular genomics at Cleveland Clinic will expand care for patients with inherited risk of cardiomyopathy, arrhythmias, lipid disorders, early heart attack and other cardiovascular diseases.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Haslam-Bailey Family Section of Cardiovascular Genomics and Precision Medicine will integrate genetic testing and counseling into routine cardiovascular care, changing how heart disease is detected, treated and prevented. In tandem, the Center for Cardiovascular Genomics and Data Science will lead research in discovery genomics, genomic risk prediction and translational science.
“We have a unique opportunity to bridge groundbreaking research and patient care, and help shape the future of precision cardiovascular medicine,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “By integrating clinical genomics and investigative studies, we can offer our patients access to the latest screening strategies and treatments tailored to their unique risks, including novel gene therapies. Whether it’s evaluating a concerning family history or participating in clinical trials, this approach ensures that patients and families are guided by the most advanced science.”
Both the clinical and research arms of this initiative will be led by Krishna Aragam, MD, Cleveland Clinic’s inaugural William E. Macaulay Endowed Chair in Cardiovascular Genomics.
Dr. Aragam joined Cleveland Clinic from Massachusetts General Hospital and the Broad Institute of MIT and Harvard, where he led NIH- and foundation-supported programs in cardiovascular genomics. His work spans gene discovery and genomic risk prediction, with leadership roles in national and international research consortia.
Advertisement
Consult QD recently spoke with Dr. Aragam about his passion for cardiovascular genomics, his research achievements and his plans for the new initiative at Cleveland Clinic.
A: Early in my medical training, I saw patients with early heart attacks without clear clinical risk factors. I saw patients with heart failure or cardiomyopathy without a clear cause. It seemed intuitive that genetics may be playing a role in these cases, but we lacked the tools to fully define the risk. At the same time, genomic science was accelerating rapidly, and population-scale studies began to reveal the specific genetic contributors underlying conditions we had long suspected were heritable.
Those early patient encounters combined with the rapidly evolving science convinced me that genomic medicine was going to help shape the future of cardiology. That’s what drew me to this field, and I’ve stayed in it because I believe genomics influences almost every domain of cardiology.
Across all conditions, our goal is to identify a patient at high risk before they have a catastrophic event — such as a heart attack, malignant arrhythmia or aortic rupture — and tailor their management to change their clinical trajectory and avoid that adverse outcome.
A: At Mass General, I trained in clinical cardiology and then in clinical and investigative cardiovascular genomics. I spent my time on faculty there identifying genetic contributors to cardiovascular disease, developing tools for genomic risk prediction and thinking about how to translate those insights into care.
Advertisement
The next step was to bring that work to a health system where it could be incorporated into clinical workflows. That requires an institutional commitment to integrating genomic science with clinical care and doing so at scale so it becomes a routine part of cardiovascular practice rather than a niche service. Cleveland Clinic leaders articulated a vision for cardiovascular genomics that aligned with mine: making genomic medicine central to how we diagnose, manage and prevent cardiovascular disease. That’s ultimately what drove my decision to come here.
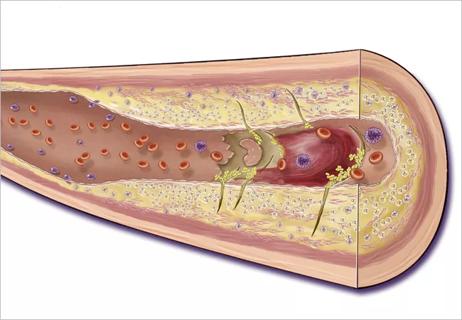
A: I’d group them into three areas. First are the large-scale discovery efforts to identify genes and variants that contribute to coronary artery disease, heart failure and dilated cardiomyopathy — often requiring international collaboration and very large datasets.
Second is developing and validating genomic risk scores that meaningfully stratify risk at the individual level (in coronary artery disease and hypertrophic cardiomyopathy, for example) and complement traditional clinical risk assessment (such as for coronary artery disease and cardiomyopathy).
Third is our team’s recent work identifying a loss-of-function variant in the gene CD36, which is common in people of African genetic ancestry and increases risk of dilated cardiomyopathy. This finding provides new insights into the mechanistic basis of disease for this population.
A: The vision is to build a comprehensive, integrated cardiovascular genomics program that spans discovery science and clinical implementation. We want to understand where genomics will have the greatest impact on patient care and acknowledge where it may not.
Advertisement
Part of this work will involve training our clinicians to practice genome-informed medicine so that it becomes embedded in routine care, with genomic testing and counseling incorporated in our standard workflows. The patients we encounter will inform the research we pursue, which in turn will inform patient care, first at Cleveland Clinic and then hopefully beyond. We see immense potential in having the clinical and research initiatives interwoven.
Another important aspect of this integrated effort is to develop the infrastructure for a health-system-associated biobank that enables prospective studies on individuals who have high genetic risk. That idea has often been described as “the future,” but we will have the scale of clinical genomics care as well as the analytic and biobanking capabilities to begin doing this in a rigorous and practical way.
A: Yes. The clinical section has been formed. We now have clinical champions within several domains of cardiovascular genetics: inherited lipid disorders and atherosclerosis, cardiomyopathy, arrhythmias, aortopathies, and other vascular conditions. These faculty members will lead their colleagues in keeping genome-guided care top of mind and incorporating it into workflows.
In addition, we are adding computational infrastructure to power our research. We are recruiting personnel to analyze the genetic data. We’re also building up genomic counseling services on both the clinical and research sides to help us translate new genomic findings into clear, practical guidance for patients and families — not just individual test results.
Advertisement
A: Historically, we’ve treated diseases as either “genetic” or “not genetic,” but most cardiovascular conditions exist on a spectrum. A single genetic finding doesn’t guarantee disease, and many people develop heart disease because genetic factors combine with clinical risk factors and life circumstances. Genomic medicine is the integration of all those layers into clinical decision-making.
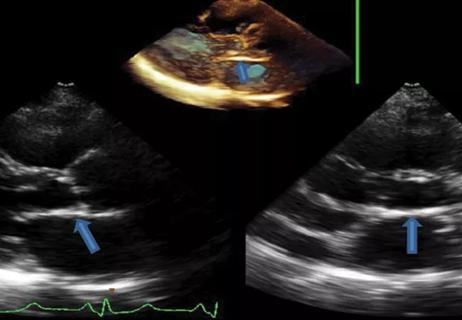
I also think it’s important for the medical community to understand that we’re looking for specific clinical situations where our current standard of care may be lacking and where research has revealed particularly strong genetic predictors. Cardio-oncology is one example. Patients with cancer who are receiving various chemotherapies, such as anthracyclines, can develop cardiac complications from those medications. Growing evidence suggests that there are genetic factors that identify which patients receiving that chemotherapy are more likely to develop systolic dysfunction. If we can identify higher-risk patients earlier, we can tailor surveillance (through echocardiograms) and, when appropriate, consider alternative regimens in partnership with oncology.
That’s the type of clinical impact we intend to make and the type of playbook we intend to write for genomic science.
Advertisement
27th offering of this CME favorite to be held March 6-9 in Hollywood, Florida

Metabolites from animal product substrates implicated in heart failure development in community cohorts

ACC committee underscores need to properly weigh benefits in risk-benefit calculations
Weakened endorsements in settings of normal EF and mild-moderate LV dysfunction may cause harm

Genetic variants exist irrespective of family history or other contributing factors

CD36 loss-of-function variant accounts for large portion of risk in this population

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Paired blood and brain tissue methylation findings raise prospect of noninvasive precision diagnosis