Risk is not trivial; finding may assist in informed decision making
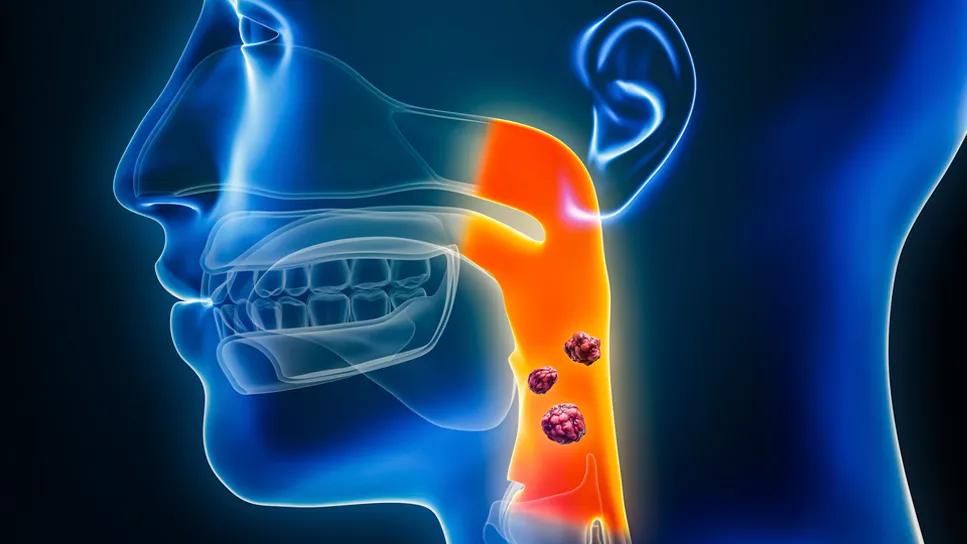
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9fccf989-2523-4fcf-9869-4264624b9411/radiation-induced-HPV-associated-oropharyngeal-cancers-1469805377)
HPV associated oropharyngeal-cancers
The 10-year cumulative incidence of radiation-induced second malignancies (RISM) among patients receiving radiation therapy (RT) for human papilloma virus (HPV)-associated cancers of the oropharynx is nearly 2%.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This finding comes from an interrogation of a Cleveland Clinic Cancer Institute database of 662 patients with cancers of the head and neck who were treated with definitive intensity-modulated RT from January 2009 to December 2020 at Cleveland Clinic. The findings were presented by Erik M. Davies, MD, resident in Radiation Oncology at Cleveland Clinic, during the 2025 American Society for Radiation Oncology (ASTRO) meeting.
Radiation is an important treatment of HPV-associated oropharyngeal cancer. “For patients with early-stage disease, these findings will enable clinicians to have a more comprehensive discussion about the risks and benefits of radiation therapy,” says Dr. Davies.
“The patient population with HPV-positive disease has a very high likelihood of cure with the right treatment. It is also a younger population who likely has decades of life ahead of them. As such, not only is the goal to cure these patients but also for them to live well for the long term. As the number of treatment options proliferates and as we start to figure out how to de-escalate therapy for select patients, we need to have a sense of the full spectrum of benefit and risk over their future lifetime. That includes risks of secondary malignancies,” adds senior study author Neil M. Woody, MD, radiation oncologist at Cleveland Clinic.
“Most broad estimates of RISM in patients receiving RT for HPV-positive head and neck cancers are obtained from population-level databases, which do not specify where the second malignancies arise in relation to the prior radiation,” says Dr. Davies.
Advertisement
For this analysis, RISM were defined as tumors occurring within the 50% isodose line of the index tumor with at least one of the following features: tumor occurring >5 years from treatment; occurrence at a geographically distinct site or subsite or a histopathologically distinct primary tumor (including HPV-negative tumors).
Using the Cleveland Clinic database allowed Dr. Davies and colleagues to follow patients longitudinally over the long term. The median follow-up for the entire cohort of patients was 58.4 months, with the longest follow-up being 160 months.
Eight patients developed a second RISM, ranging from 19.4 to 140.0 months after receiving RT. The cumulative incidence of RISM was 0.37% at five years and 1.74% at 10 years. All eight RISM were pathologically lymph node negative.
Of the eight who developed an RISM, five of the index tumors receiving RT were located in the tonsil, two in the base of tongue and one on the soft palate. In these eight patients, RT prescriptions ranged from 70-74 Gy, and six patients received concurrent chemotherapy. Seven of the eight patients received RT to the bilateral neck regions, with one receiving RT to the ipsilateral neck. RISM occurred at subsites distinct from the index tumor in seven of the eight patients. All eight patients with RISM underwent treatment with surgery that included neck dissection.
The five-year overall survival (OS) of the entire HPV-positive patient cohort receiving intensity modulated RT was 83%, and 10-year OS rate was 69%. A total of 109 of the 662 (16.6%) patients had disease recurrence, indicating that the risk of RISM remained substantially lower than the risk of tumor recurrence.
Advertisement
If HPV-positive head and neck cancers are caught early enough, patients may be good candidates for surgery and omission of RT, says Dr. Davies. “Based on our data, a patient in the early stages might preferentially be recommended for surgery.” However, patient selection is crucial and a surgical and radiation team is needed, and as Dr. Woody notes, “some robotic surgery patients may need chemotherapy and RT afterward anyways to obtain optimal cancer cure rates.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting