Recommendations focus on selecting the right biomarkers for the right setting
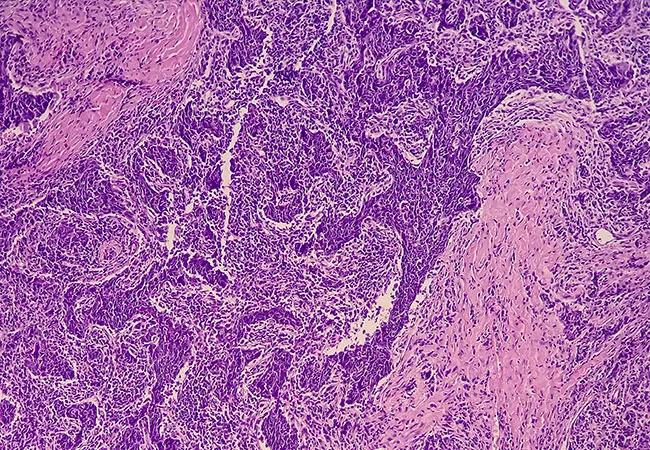
An estimated 66,470 people in the U.S. were diagnosed with head and neck squamous cell carcinoma (HNSCC) last year. These encompass a varied and complex set of diseases that often are diagnosed at an advanced stage. Many HNSCC treatments can significantly impact a patient’s quality of life, causing issues with speech, taste, swallowing, lymphatic processes and more, making it all the more crucial to hone in on the right targeted therapy from the start. Clinicians often struggle with determining the optimal frontline treatment and choosing between immunotherapy and more systemic therapies in recurrent metastatic disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With the emergence of immune-checkpoint inhibitors for use frontline treatment of head and neck cancers, biomarkers such as programmed death ligand-1 (PD-L1) and tumor mutation burden are increasingly important for treatment selection. To that end, ASCO convened a panel of medical, surgical and radiation oncologists as well as radiology, pathology and patient advocacy experts to create a single source of information for treating recurrent disease in different types of head and neck cancers. A patient representative also played a significant role in developing the recommendations, ensuring that the guidelines were practical and that the language was accessible to patients.
“We wanted to provide clearer guidelines to clinicians and patients for all range of head and neck cancers, including less common cancers such as nasopharyngeal carcinomas and salivary gland tumors,” says Emrullah Yilmaz, MD, PhD, expert panel co-chair and a hematologist/oncologist with Cleveland Clinic’s Taussig Cancer Institute. “Particularly for rare cancers, where there are not large sets of trial data, it can be tough to know which treatment approach to use.”
To produce the guidelines, the panel conducted an extensive review of 28 relevant phase 3 trials published between 2000-2022 to discern outcomes of interest, such as survival and overall response to treatment. “The most important takeaways from the new ASCO guidelines are to check the patient’s PD-L1 to help with the decision about whether to use a single agent or combination immunotherapy, with or without chemotherapy,” says Yilmaz.
Advertisement
Notable updates to the ASCO guidelines include the following recommendations:
The panel hopes that guidance for more specific treatments will result in higher success rates for patients. Dr. Yilmaz noted that there is more work to be done to continue to develop appropriate therapies. “Participation in ongoing clinical trials will help to further improve outcomes. There is much effort being undertaken by the National Cancer Institute to design trials that are easier for patients to participate in.”
Advertisement
Learn more in our recent podcast.
Advertisement
Advertisement

Combination therapy demonstrates effectiveness in first-line treatment setting

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Genetic variants exist irrespective of family history or other contributing factors

Why Cleveland Clinic is launching its cardioimmunology center

Percutaneous stabilization can increase mobility without disrupting cancer treatment

Collaborative patient care, advanced imaging techniques support safer immunotherapy management