New research demonstrates that cfDNA methylation patterns may noninvasively identify tumor hypoxia in head and neck squamous cell carcinoma
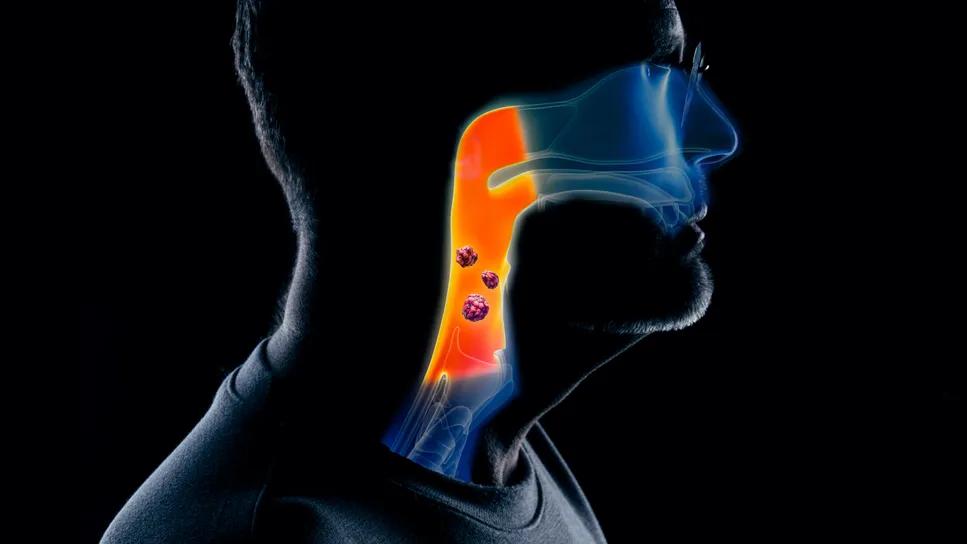
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3c4b32e0-152f-4af9-8a7a-854524f951a3/inferring-intratumoral-hypoxia-1302515665-1469805377)
Head and neck cancer illustration
A novel blood-based assay may offer a noninvasive and longitudinal method to identify tumor hypoxia to guide future treatment de-escalation for patients with HPV-associated head and neck squamous cell carcinoma (HNSCC). In research presented at the 2025 American Society for Radiation Oncology (ASTRO) Annual Meeting, investigators demonstrated that hypoxia-associated methylation signatures in circulating tumor DNA (cfDNA) are detectable in pre-treatment plasma and may reflect intratumoral gene expression.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Promoter methylation was observed in hypoxia-responsive genes. Targeted bisulfite sequencing could provide a noninvasive approach to infer bulk intratumoral gene expression for mechanistic and dynamic insights,” according to the Cleveland Clinic-led research team.
The findings support the potential for a precision medicine approach to treatment stratification, especially in a population where cure rates are high but standard therapy comes with significant toxicity.
“We’re trying to move away from a one-size-fits-all model,” says study author Jacob Miller, MD, a radiation oncologist specializing in the treatment of head/neck and gastrointestinal cancers at Cleveland Clinic Cancer Institute. “The standard is seven weeks of concurrent radiation and chemotherapy, and while most patients are cured, the side effects are substantial. If we can personalize treatment based on tumor biology, we could maintain outcomes and reduce toxicity.”
While HPV-positive oropharyngeal cancers are often highly curable, a persistent clinical dilemma remains: most patients endure significant toxicity from the standard seven weeks of chemoradiotherapy, but clinical trials suggest that a small subset of patients require this full regimen to achieve a cure. Identifying which tumors are more resistant to treatment is critical, but current approaches relying on traditional clinical and imaging factors fall short.
“Over the last 20 years, clinical trials in this disease have shifted from increasing the cure rate—which is already high—to reducing the intensity of treatment. The goal has been to maintain cure rates while minimizing side effects,” says Dr. Miller. “However, most de-escalation trials have shown that simply reducing treatment across the board—for example, cutting radiation from seven to six weeks or switching chemo—can reduce the cure rate. This suggests that while many patients could be cured with less treatment, there’s a subgroup whose tumors are more resistant and still require the full course.”
Advertisement
Pre-treatment intratumoral hypoxia is a well-established prognostic and predictive biomarker for response to chemoradiotherapy in HNSCC, including HPV-positive oropharyngeal cancers. Hypoxia contributes to treatment resistance, and patients with more hypoxic tumors may require the full course of therapy, while others could potentially benefit from de-escalation. However, current methods to assess hypoxia, such as 18F-FMISO PET imaging, are not widely available, and tissue-based gene expression profiling has limitations due to tumor heterogeneity, RNA degradation, and the inability to dynamically assess changes over time.
To address this gap, Dr. Miller and his team hypothesized that hypoxia could be inferred noninvasively through blood—specifically, by using targeted methylation sequencing of circulating tumor DNA (cfDNA). “We wanted to know if we could detect tumor hypoxia in a blood-based test,” he says.
In this analysis, the investigators designed a custom plasma targeted bisulfite sequencing assay to capture tumor-associated cfDNA among patients with HNSCC. “The purpose of bisulfite conversion is to measure methylation in specific target regions associated with hypoxia,” Dr. Miller explains.
The targeted panel included 257 differentially methylated regions (DMRs) from the validated Hypoxia-M methylome classifier (31.1 kb), 790 human DMRs in 13 additional HPV dysplasia- or hypoxia-associated genes (95.6 kb), and seven high-risk HPV genomes (16, 18, 31, 33, 35, 45, 52, 47.4 kb), spanning a total of ~12,100 CpG sites.
Advertisement
To ensure comprehensive enrichment, four hybridization probes were included per target region, capturing both DNA strands and both methylated and unmethylated bisulfite-converted, adapter-ligated cfDNA fragments.
Pre-treatment plasma samples from 12 patients with HNSCC—seven with HPV16-positive tumors and five with HPV-negative tumors—were analyzed using the custom targeted bisulfite sequencing assay.
All patients underwent definitive radiotherapy, with most receiving concurrent platinum-based chemotherapy (n=10). The cohort represented predominantly advanced-stage disease, with 75% (9 of 12) presenting with AJCC8 cT3-4 or cN2-3 tumors. Median plasma HPV16 DNA concentration was 30.5 cp/mL among HPV+ tumors. A median 15% (range, 11-21%) of hypoxia DMRs were hypomethylated and 20% (19-25%) were hypermethylated, according to the study authors.
“This was a diagnostic validation study, so our main goal was to demonstrate test performance,” Dr. Miller notes. “We verified that the sequencing platform was able to enrich methylated and unmethylated cell-free DNA fragments in plasma, both associated with the human genome and the viral genome.
“We then took a representative cohort of patients in a small pilot and found that the test accurately distinguished HPV-positive and HPV-negative individuals,” he adds. “We observed distinct methylation patterns in the hypoxia-related genes. For example, one gene called STC2, which plays a role in the hypoxia pathway, was consistently hypermethylated (i.e., silenced) before treatment. Other genes—like VEGFA, HIF1 and CA9, both well-established in hypoxia literature—were hypomethylated (i.e., active) in patients who later experienced disease recurrence.”
Advertisement
The results of this study demonstrate the potential of a novel, blood-based methylation assay to noninvasively assess tumor hypoxia in patients with HNSCC. The approach could provide mechanistic and dynamic insights while complementing hypoxia PET imaging or tissue-based profiling.
Dr. Miller and his team are now expanding the study to include approximately 100 patients with HPV-positive HNSCC, with plans to conduct longitudinal testing across treatment. The next goal would be to compare how well this approach performs against tissue-based tests.
In the long term, Dr. Miller hopes to change how these patients are treated. “If we find that this diagnostic performs well and accurately, we could develop a clinical trial to assess if a more personalized approach can maintain cure rates while decreasing side effects and improving quality of life,” he concludes.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches