Proof-of-concept study finds technology improves quantitative evaluation of blood flow characteristics
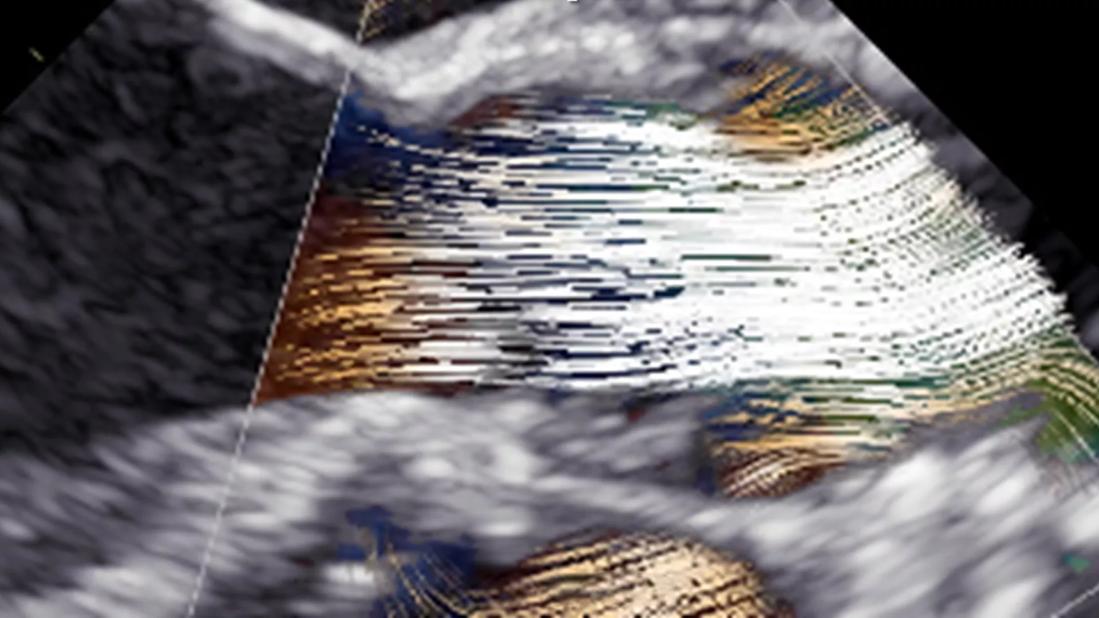
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a546eef5-21e0-4b00-ba5d-149c6c73e065/blood-speckle-imaging)
blood speckle imaging of the aortic valvar leaflets
Assessment of aortic valvar hemodynamics is essential to optimize outcomes for patients undergoing surgical repair of their aortic valve. This assessment is typically limited to peak blood flow velocity measured preoperatively and postoperatively with Doppler echocardiography, and color flow mapping which allows crude visualization of blood flow direction.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Results of a pilot study by Cleveland Clinic researchers and colleagues from the KTH Royal Institute of Technology in Stockholm, Sweden, suggest that a new technology – blood speckle imaging (BSI) – has potential to generate more detailed evaluation of blood flow characteristics, including accurate estimates of wall shear stress in patients with forms of aortic valvar and subvalvar disease. The results were published in Bioengineering.
“We used BSI with a newly available mini-4D transesophageal probe to assess more detailed blood flow characteristics in a pediatric patient undergoing subaortic membrane resection and aortic valve repair,” says Justin T. Tretter, MD, senior author of the study and Co-Director of the Congenital Valve Procedural Planning Center. “BSI underpredicted aortic root peak velocities preoperatively in those with stenosis, but it had high agreement with Doppler echocardiography postoperatively once the stenosis is relieved. We were able to compare more detailed preop and postop blood flow velocity profiles, which is not possible with Doppler.”
Blood speckle imaging involves tracking speckles that occur as blood cells move from one frame of an image to the next. A “best match” search algorithm is used to create blood vector velocity patterns of the speckles, which are captured at ultra-high frame rates. Unlike color Doppler, BSI requires neither contrast agent injection nor mathematical assumptions.
“With Doppler, depending on the type, we can generate a very generalized color map of the direction of blood flow or visualize velocity along the ultrasound beam or in a localized area,” says Dr. Tretter. “BSI takes the mapping to another level, allowing us to look in very specific detail at vector blood flow patterns across an entire 2D echocardiographic image, estimate the resulting stresses experienced by the aortic valvar leaflets and aortic walls, potentially aiding in pre and postoperative decision-making.”
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/56d35344-22e8-48bb-85dc-3eab5e2a8ba2/blood-speckle-imaging-inset)
Figure. An example of blood speckle imaging before and after resection of a subaortic membrane with repair and rehabilitation of the aortic valvar leaflets demonstrates improved, laminar blood flow during systole.
The patient in the pilot study was a child who underwent standard surgical resection for recurrent subaortic membranes. Extensions of the membranes were peeled from under the ventricular-facing surface of all three aortic valvar leaflets. Transesophageal imaging performed intraoperatively revealed satisfactory resection with no significant aortic valvar regurgitation or stenosis.
Preoperatively and postoperatively, BSI images were obtained with an ultrasound system and transesophageal probe.
The preoperative images revealed abnormal blood flow patterns and high peak velocity associated with obstruction of left ventricular outflow and restricted valvar leaflets. With resulting resolution of stenosis and only trivial regurgitation, the postoperative BSI assessment, in contrast, showed improved, more laminar hemodynamic patterns and improved shear stress both on the leaflets and aortic walls.
From a statistical perspective, the confidence levels for the postoperative BSI measurements in the aortic root were higher, whereas the preoperative confidence levels were relatively lower and less uniform. This relates to the current limitation in accuracy of BSI assessment at higher blood flow velocities.
“We used BSI data in this clinical case to retrospectively analyze flow patterns and derived properties to visually assess and quantify the hemodynamic changes from surgery,” says Dr. Tretter. “The imaging confirmed that wall shear stress on the anterior aspect of the aorta was reduced after correction of the asymmetric systolic antegrade jet.”
Advertisement
BSI is now being performed on every patient who undergoes screening at the Congenital Valve Procedural Planning Center, along with standard echocardiographic imaging, to further understand the applications of this additional hemodynamic data. The authors emphasize, however, that before the technology can be implemented more widely, larger studies are needed to validate their findings and standard protocols for clinical use of BSI must be developed.
“BSI has decreased accuracy in patients with stenotic valves because of the very high blood flow, but the technology is very promising in the population with leaky valves and may allow us to do a better job of saving those aortic valves,” says Dr. Tretter.
The researchers hope that BSI may ultimately help them assess and predict the durability of aortic valvar repairs over the short and long term, allowing them to fine-tune the procedures and improve patient outcomes.
“We’ve just begun to explore the use of BSI to quantify the turbulence of blood flow in the aorta and the stress and strain it exerts on the aortic valvar leaflets,” says Dr. Tretter. “We’re very interested in applying our findings to guide and tailor not only aortic valvar surgeries, but also treatment of other types of congenital heart disease.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
Surgeons credit good outcomes to experience with complex cases and team approach
For many patients, repair is feasible, durable and preferred over replacement
In experienced hands, up to 95% of patients can be free of reoperation at 15 years
Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach