Large retrospective study supports its addition to BAV repair toolbox at expert centers

Cleveland Clinic researchers have demonstrated that adding a figure-of-8, “hitch-up” stitch to conventional bicuspid aortic valve (BAV) repair methods is safe and achieves good long-term outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a study published in JTCVS Techniques (Epub 2024 Jan 22), they found that patients undergoing BAV repair with the figure-of-8, hitch-up stitch at commissures had low operative mortality as well as similar valve durability and survival at 10 years compared with patients who underwent BAV repair without the figure-of-8 stitch.
“Our data suggest that the figure-of-8, hitch-up stitch can be safely added to increase the likelihood of durable BAV repair when standard techniques are insufficient,” says senior author Lars Svensson, MD, PhD, Chief of Cleveland Clinic’s Heart, Vascular & Thoracic Institute.
About 1% to 2% of the population is born with a BAV, which often leads to premature aortic valve dysfunction. For younger patients, valve repair is preferred over replacement to avoid the need for lifelong anticoagulation. However, BAV repair is more challenging than repair of a tricuspid aortic valve.
“When the patient’s anatomy permits, valve repair is the first option for treating BAV regurgitation at centers with the requisite surgical expertise,” Dr. Svensson says. However, because prolapse of the fused cusp is almost always present in these cases, correction of the prolapse without compromising the opening of the bicuspid valve is critical.
Dr. Svensson notes that traditional options for addressing cusp prolapse can have limitations. For instance, free margin plication is sometimes insufficient to address cusp prolapse since the extension of plication must be limited to reduce the likelihood of stenosis. Another option, triangular cusp resection, has been associated with inferior valve durability.
Advertisement
In contrast, the figure-of-8, hitch-up stitch offers potential advantages over these methods. Because higher coaptation is needed for a durable BAV repair in most cases, the figure-of-8, hitch-up stitch promises durability benefits by elevating the commissures to reinforce valve closure. Moreover, it can move a commissure in the direction opposite to a prolapsing cusp when necessary. And by increasing tension of a prolapsing leading edge, the technique can be especially protective against prolapse in cases of valve-sparing aortic root reimplantation.
For these reasons, Cleveland Clinic has used the figure-of-8, hitch-up stitch for BAV repair since 2006. Briefly, the technique involves placement of a polytetrafluoroethylene (PTFE) stitch over the leading edge of the cusps at commissures. Then sutures are passed 3 to 4 mm above the commissures approximately 3 to 4 mm apart and tied outside over a pledget.
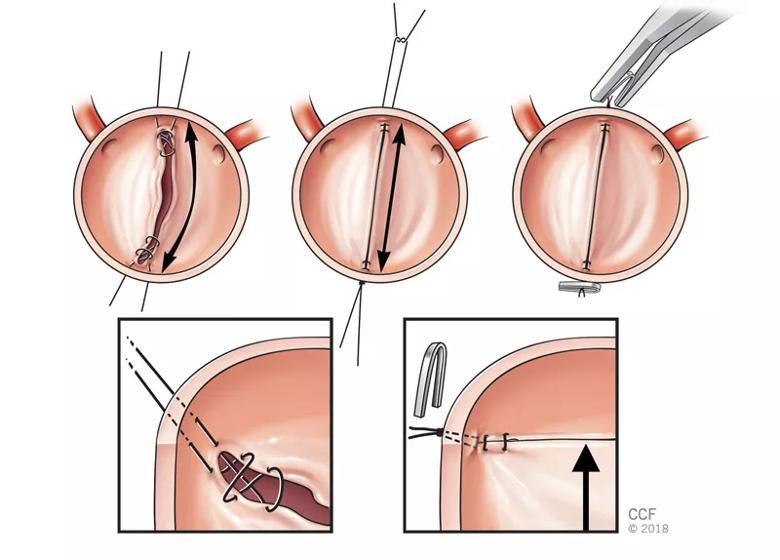
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5fb651d0-8c46-4b0e-9293-896b7a7f6fc2/bicuspid-aortic-valve-repair2)
Illustrations showing BAV repair with the figure-of-8, hitch-up stitch. This technique increases the area of apposition for the valve leaflets and elevates them to achieve more tension. The result is greater contact area and apposition, which may provide redundancy if the leaflets stretch over time.
“Previous data from our group (Ann Thorac Surg. 2018;105:739-748) suggested that figure-of-8, hitch-up stitches may enhance BAV repair durability,” Dr. Svensson says. “However, concerns around durability and safety have persisted, particularly about the risk of commissural tear and resulting effects on aortic valve gradient. We undertook this analysis to better characterize early and long-term outcomes with this technique.”
Dr. Svensson and colleagues reviewed prospectively collected outcomes data among 1,112 patients who underwent BAV repair at Cleveland Clinic from 2000 to 2022. Of these patients, 367 underwent BAV repair with the figure-of-8, hitch-up stitch along with conventional repair techniques like commissuroplasty and cusp plication. The figure-of-8, hitch-up stitch was used according to surgeon preference or when repair was not feasible with traditional methods.
Advertisement
These 367 patients were compared with the remaining 745 others who underwent BAV repair without the figure-of-8 technique. Propensity score matching yielded 195 well-balanced pairs for comparison.
Operative mortality was low in both the figure-of-8 cohort (0.3%) and the matched comparator group (0%). The figure-of-8 cohort had shorter bypass and cross-clamp times. At 10 years, the prevalence of moderate or severe aortic regurgitation on transthoracic echocardiography was statistically comparable between the two groups. Risk of reoperation and survival at 10 years were also similar between the groups.
The study should reassure surgeons and cardiologists about the safety of the figure-of-8 technique, notes study co-author Milind Desai, MD, MBA, Medical Director of Cleveland Clinic’s Aorta Center. “We did not observe a significant increase in risk of cusp tear or accelerated valve degeneration with this addition to the repair toolbox,” he says.
Dr. Svensson adds that the findings build on previous positive reports about the figure-of-8, hitch-up stitch from his Cleveland Clinic group and others. He says the technique is now routinely used at Cleveland Clinic when additional BAV repair techniques are needed to correct cusp prolapse and increase leaflet coaptation.
“Our data suggest the figure-of-8, hitch-up stitch can safely facilitate BAV repair when added to standard techniques, achieving good long-term outcomes,” Dr. Svensson concludes. “In experienced centers, it is a valuable tool to increase successful, durable BAV repair in patients with challenging valve pathologies. We look forward to continued monitoring to assess its impact on valve durability over even further follow-up.”
Advertisement
Advertisement
Advertisement

Experience-based takes on valve-sparing root replacement from two expert surgeons

30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward

Surgeons credit good outcomes to experience with complex cases and team approach

For many patients, repair is feasible, durable and preferred over replacement

In experienced hands, up to 95% of patients can be free of reoperation at 15 years

Experience and strength in both SAVR and TAVR make for the best patient options and outcomes

Ideal protocols feature frequent monitoring, high-quality imaging and a team approach

20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation