For many patients, repair is feasible, durable and preferred over replacement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3850db5e-37e0-47b0-9958-dd6c0f462525/bicuspid-aortic-valve-repair)
figure-of-8-shaped surgical stitch
At many heart centers, surgical valve replacement remains the standard of care for patients with significant valvular aortic regurgitation (AR), for whom no good transcatheter options exist. Over the past two decades or more, however, Cleveland Clinic has demonstrated that aortic valve repair is a safe, effective and durable option for many of these patients, particularly those younger than 65.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Repair holds a number of advantages over replacement in this setting:
“At Cleveland Clinic, we’ve performed over 3,500 aortic valve repairs to date,” says cardiothoracic surgeon Lars Svensson, MD, PhD, Chief of Cleveland Clinic's Heart, Vascular and Thoracic Institute. While that includes many hundreds of valve-sparing aortic root replacements to address concurrent aortic disease, the majority of repairs involve solely the valve for treatment of AR. These are performed as minimally invasive keyhole operations.
“We’ve shown that, at experienced centers, valve repair is effective and durable for treating AR,” Dr. Svensson says. “But only a small number of centers across the U.S. will attempt aortic valve repairs, as these procedures require a steady number of cases to maintain expertise and skills.”
Dr. Svensson points to several Cleveland Clinic publications to underscore the effectiveness and durability of aortic valve repair.
A study of 1,009 patients who underwent aortic valve repair from 2001 to 2011 found 90% freedom from aortic valve reoperation and 83% survival at 10 years after repair (Ann Thorac Surg. 2018;105[3]:739-748). These repairs involved various techniques, including cusp repair with commissuroplasty in nearly half of cases as well as commissural figure-of-8 suspension sutures, debridement, free-margin plication or resection, and annulus repair with resuspension, root reimplantation or root remodeling. This large series yielded at least two key insights:
Advertisement
While many patients in the above series had a trileaflet aortic valve, nearly comparable results can be achieved in patients with a bicuspid aortic valve (BAV). Dr. Svensson and colleagues reported long-term outcomes in 728 patients (mean age, 42 years) who underwent BAV repair at Cleveland Clinic from 1985 to 2011 (Ann Thorac Surg. 2014;97:1539-1548). Freedom from aortic valve reoperation at 10 years was 78%, and survival at 10 years was 94%. Hospital mortality was 0.41%.
“This study period stretched over 26 years,” Dr. Svensson observes. “Outcomes improved over time as we gained experience, learning how to better select patients for repair and choose which components of the operation to perform, and as we began to routinely employ the CLASS schema.” Results improved to 91% freedom from reoperation at 10 years for isolated BAV repairs, he notes.
One of the key lessons learned was the value of including a figure-of-8 hitch-up stitch among conventional BAV repair methods. “We now use this stitch at commissures in virtually all aortic valve repairs, whether BAV or trileaflet,” says Dr. Svensson, who developed the technique. The rationale is to enhance repair durability by elevating the commissures to reinforce valve closure, as illustrated in the Figure.
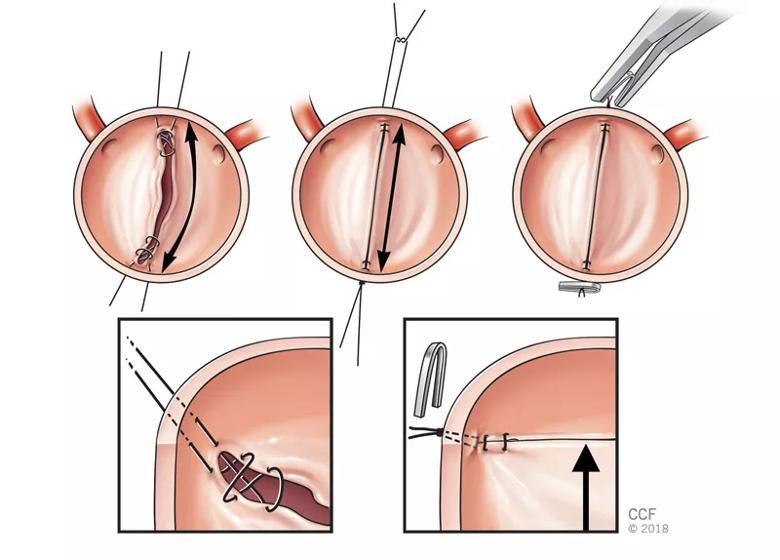
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5fb651d0-8c46-4b0e-9293-896b7a7f6fc2/bicuspid-aortic-valve-repair2)
FIGURE — Illustrations showing BAV repair with the figure-of-8 hitch-up stitch. This technique increases the area of apposition for the valve leaflets and elevates them to achieve more tension. The result is greater contact area and apposition, which may provide redundancy if the leaflets stretch over time.
A recent Cleveland Clinic study confirmed the safety of the stitch and the ability to use it for severe BAV regurgitation (JTCVS Techniques. 2024;24:27-40). That report compared early and later outcomes between two matched groups of 195 patients each undergoing BAV repair — one group with conventional repair techniques alone (e.g., commissuroplasty and cusp plication) and the other with conventional techniques plus the figure-of-8 hitch-up stitch. Operative mortality in the figure-of-8 stitch group was low (0.3%), and 10-year freedom from reoperation was comparable to that in the conventional group (80% vs. 81%), as was 10-year survival (99.5% vs. 94.6%, respectively).
Advertisement
Another notable technique Cleveland Clinic surgeons occasionally use for aortic valve repair is known as the tailoring operation, in which the intercommissural angle is narrowed with a Cabrol stitch, after which the sinutubular junction is downsized. Figure-of-8 hitch-up stitches are often placed on top of the commissures as well, to increase the area of apposition. “We tend to use this in elderly patients, with excellent long-term freedom from reoperation,” Dr. Svensson says.
Beyond surgical expertise, optimal AR management demands well-informed vigilance in disease detection as well. “Patients with severe AR often remain asymptomatic for a very long time, yet a number of studies show that subclinical left ventricular myocardial dysfunction occurs early in the compensated stage with preserved left ventricular ejection fraction, before overt symptoms develop,” says Milind Desai, MD, MBA, Medical Director of Cleveland Clinic’s Aorta Center and a cardiologist in its Valve Center. “Recent years have seen recognition that patients can benefit from surgery at this stage.”
To identify patients at this stage, Dr. Desai and his colleagues often rely on multimodality imaging that begins with transthoracic echocardiography. “A quality echo is absolutely needed,” Dr. Desai says. “But often in patients with AR, the jet is eccentric, which can cause underestimation of the degree of AR. In many of those cases, we will add transesophageal echocardiography (TEE) or cardiac MRI, particularly when there is discrepancy between what we’re seeing in terms of severity of valve regurgitation and size of the left ventricle. While TEE, including 3D TEE, is particularly helpful for recognizing the etiology and ascertaining the severity of AR, MRI can help quantify AR and, more importantly, provide a precise assessment of LV volumes and ejection fraction.
Advertisement
“Many of these patients will have aortopathy,” he continues. “If we suspect aortopathy, a gated tomographic scan like contrast-enhanced CT or MRI is helpful to allow precise measurements. And CT is valuable for identifying significant calcification, which will rule out repair.”
Once AR requiring intervention is confirmed, Dr. Desai becomes even more focused on determining whether the patient’s anatomy is conducive to valve repair. “Every patient we refer for repair is told we will attempt repair but there’s a chance the surgeon may have to replace the valve based on what’s seen in the operative field,” he says. “I advise patients younger than 45 or 50 to be prepared for the possibility of a mechanical valve unless we identify in advance a compelling reason to go with a bioprosthesis if repair isn’t feasible.”
In fact, Dr. Desai sees the nimbleness of his surgical colleagues as a leading asset for patients seeking the best solution for their AR at Cleveland Clinic. “Aortic valve repair is a sophisticated operation that should only be attempted by deeply experienced surgeons who have performed plenty of these repairs before,” he says. “We have a highly competent group of surgeons who, even with their experience, are not just aortic valve repair specialists. They are highly versatile surgeons who can respond to the patient’s valve anatomy in the moment and do whatever is needed to take the patient out of harm’s way.”
He adds that these surgeons are backed by highly experienced cardiologists “who have seen enough to be able to tell a patient, when necessary, ‘Unfortunately, repair is not going to work here. Replacement will be a much better option, based on solid imaging evidence.’ That’s what we owe our patients.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
Surgeons credit good outcomes to experience with complex cases and team approach
In experienced hands, up to 95% of patients can be free of reoperation at 15 years
Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach
20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation