Ophthalmologists’ prompt diagnosis can help improve patients’ quality of life

Cancer metastases to the eye are rare, but they are becoming more prevalent as patients live longer following cancer diagnosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Breast cancer and lung cancer are the metastatic diseases we most often see in the eye,” says Arun D. Singh, MD, Director of Ophthalmic Oncology at Cleveland Clinic Cole Eye Institute. “That may be because those cancers are most prevalent in the general population. Colon, prostate and skin cancer also can metastasize to the eye. Rarely do we see sarcomas.”
While oncologists direct treatment of metastatic disease, ophthalmologists can help with diagnosis, he says. Metastases most commonly appear in the uvea and orbit — rarely in the retina and vitreous. They can manifest as ocular motility issues, pain, double vision, sunken or bulging eyes, or other ophthalmic conditions.
Dr. Singh explained more about the diagnosis and treatment of eye metastases in a recent episode of Cleveland Clinic’s Cancer Advances podcast.
Symptoms of a metastasis to the uvea or elsewhere in the globe often involve some kind of visual distortion, such as a shadow in the field of vision or a general loss of vision. Metastases to the orbit can cause double vision, difficulty moving the eye or a change in positioning of the eye. Rarely metastases can mimic inflammation.
“If the eye is red, painful and not responding to treatment, it may be a metastasis masquerading as inflammation,” notes Dr. Singh.
Cancer therapies, themselves, can cause vision changes, he adds. However, if a patient is concerned enough to report a visual complaint, their eyes should be examined.
Metastases may not appear on conventional MRI or CT scans because the eye is so small. But ophthalmologists can view potential metastases with standard ophthalmic equipment and then order eye ultrasounds, optical coherence tomography or other imaging as needed.
Advertisement
Biopsy of the eye may be necessary if metastasis is suspected but the patient has no evidence of metastatic disease elsewhere.
“If the patient has been diagnosed with metastatic disease and now has vision changes, a biopsy is not needed,” says Dr. Singh. “Clinical findings alone can be corroboratory.”
When an eye metastasis is diagnosed, it’s important for an oncologist to assess the patient’s current cancer therapy.
“Even though the eye is an extension of the brain, the uvea doesn’t have a blood-brain barrier,” says Dr. Singh. “Intravenous cancer therapies will access tumors in the choroid or uvea, which have circulation like the rest of the body. So, if metastases are still occurring there despite primary cancer therapy, it’s time to explore alternative treatment” (Figures 1 and 2).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/57f5f498-2b93-4995-bc8f-b13a38e83c06/23-EYE-3665374-Cancer-metastasis-Inset-1A_jpg)
Figure 1. A 58-year-old woman presented with blurry vision in the left eye over three weeks. She had history of metastatic breast cancer (brain, skin, spine, pancreas, adrenal gland, lung, lymph nodes, thyroid) following mastectomy. Examination revealed a yellow choroidal lesion inferotemporal to the macula, measuring 12 mm by 5 mm by 1.5 mm.
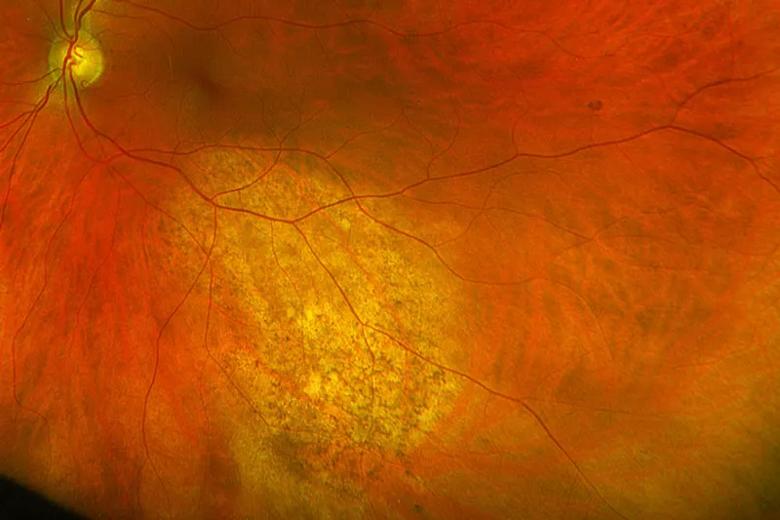
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8523a7dc-72aa-44f0-8b6b-9c12ab907e6d/23-EYE-3665374-Cancer-metastasis-Inset-1B_jpg)
Figure 2. Within four weeks of treatment with gemcitabine, carboplatin and pembrolizumab, partial regression of the tumor was evident. At three months, tumor regression was complete with only chorioretinal atrophy observed at the site.
If second-line therapies are not available, radiation therapy may be considered. However, metastases can be multifocal, making it challenging to treat each spot.
For carcinoid tumors and other tumors for which there aren’t effective chemotherapies, laser treatments are available.
Eye metastases may not be top of mind for ophthalmologists, but they do occur, and they do warrant prompt care. The sooner the metastasis is addressed and the sooner the patient’s vision is improved, the better the patient’s quality of life.
“Vision complaints may be the only sign of cancer that a patient experiences on a daily basis,” says Dr. Singh. “As long as the patient is alive and blinking, they are constantly being reminded of their diagnosis. We need to be mindful of that and be empathetic. Addressing cancer metastasis to the eye is primarily about improving a patient’s quality of life.”
Advertisement
Advertisement

Registry data highlight visual gains in patients with legal blindness

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

The advanced stage of diabetic retinopathy is among the most challenging for retinal surgeons

Evidence mounts that these diabetes and obesity drugs may protect eyes, not endanger them

It’s the first step toward reliable screening with your smartphone

CFH gene triggers the eye disease in white patients but not Black patients

Study identifies factors that may predict vision outcomes in diabetic macular edema

Fixational eye movement is similar in left and right eyes of people with normal vision