New study validates bone-salvaging technique in shoulder surgery

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/98aded95-7b9d-4be9-b1c8-aa1fecba6c60/19-ORT-1452-Shoulder-CQD-Hero_jpg)
19-ORT-1452-Shoulder-CQD-Hero
A recent proof-of-concept study published in the Online Journal of Shoulder and Elbow Surgery demonstrated the clinical utility of a surgical technique for patients undergoing a total shoulder arthroplasty (TSA). The study validated a technique that has seen greater demand in recent years — first from professional weightlifters and serious athletes and now from a more general patient population in need of a shoulder replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Anthony Miniaci, MD, a shoulder and sports medicine surgeon in Cleveland Clinic’s Department of Orthopaedic Surgery and senior author of the study, notes that this technique is a paradigm shift for shoulder surgery.
“It’s less invasive because it’s bone preserving,” he says. “Most patients who receive this surgery tend to recover very quickly. Depending on the circumstances, they may be discharged the same day or next day.”
The technique is based on a two-part concept designed to more accurately mimic the anatomy of a patient’s humeral head and also use inlay technology that is less invasive and salvages more of the patient’s bone.
The humeral component of the replacement is traditionally shaped like a sphere even though anatomically the humeral head is more of an ovoid shape. While using an ovoid-shaped replacement has shown promising results in laboratory studies, this study validates these findings in a clinical setting.
On the glenoid side, where onlay replacement is traditionally used, Dr. Miniaci and his team combined the humeral head replacement with an inlay implant. Instead of gluing the plastic on top of the bone, the surgeons make a little slot for it in the bone, so that it takes some stress off the plastic.
Dr. Miniaci first conceptualized this technique after observing an unmet need in the patient population he was treating, many of them athletes. He was so pleased with the outcomes that he began to use this approach for every shoulder replacement.
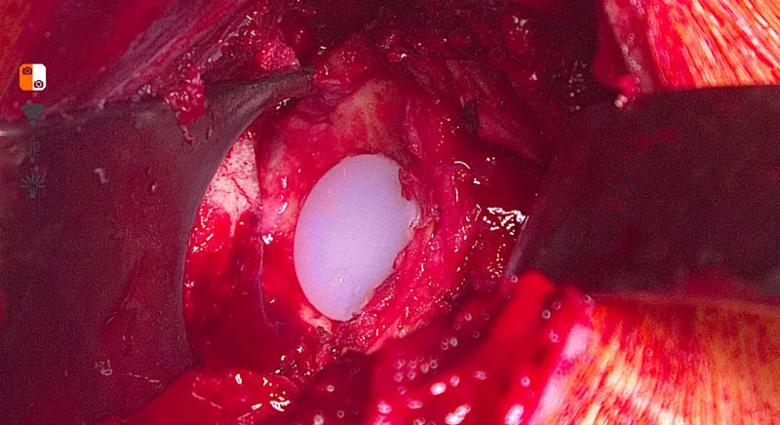
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c9e829bf-20dd-4bbc-8aa6-be3b7cd3c4c1/19-ORT-1452-Shoulder-CQD-Inset-3_jpg)
The inlay implant is slotted into the bone so that it shares stress with the patient’s own glenoid.
Advertisement
This retrospective study examined 31 shoulders in 29 patients (25 males, 86.2%; 4 females, 13.8%) with an average age of 58.5 years and mean follow-up of 42.6 months. All patients received a preoperative diagnosis of osteoarthritis and were treated with a combination approach of nonspherical humeral head and inlay glenoid replacement by a single surgeon from 2011 to 2016.
In the two groups, one with preoperative concentric glenoids (N = 7) and one with nonconcentric glenoids (N = 24), there were no significant differences in patient-reported outcomes including pain relief, function and satisfaction. The technique showed positive outcomes despite differences in glenoid morphology.
“This is important because while TSA has proved an effective therapeutic approach to treating pain and improving function, there are relatively little data to compare outcomes for concentric and eccentric glenoids,” remarks Dr. Miniaci. “This study helps confirm that we can sensibly use this approach for patients with concentric or eccentric glenoids.”
The comparison of preoperative with postoperative range of motion also showed a significant improvement in forward flexion. All patients with baseline Penn scores surpassed the 30% clinically important difference threshold on their maximal possible improvement, and 94% met or exceeded the
substantial clinical benefit mark.
This proof-of-concept study is a first step in validating the procedure’s clinical success. Dr. Miniaci hopes it soon becomes a standard operation for all patients in need of TSA.
Advertisement
“This technique has the potential to alter the standard of care for treating TSA. I am eager to continue exploring this approach and even less-invasive options to treat future patients,” he says.
Dr. Miniaci reports that he receives financial support (consultant fees, speaker fees, honorarium, royalties, stock options) from Arthrosurface, Inc. and Trice Orthopedics, Inc.
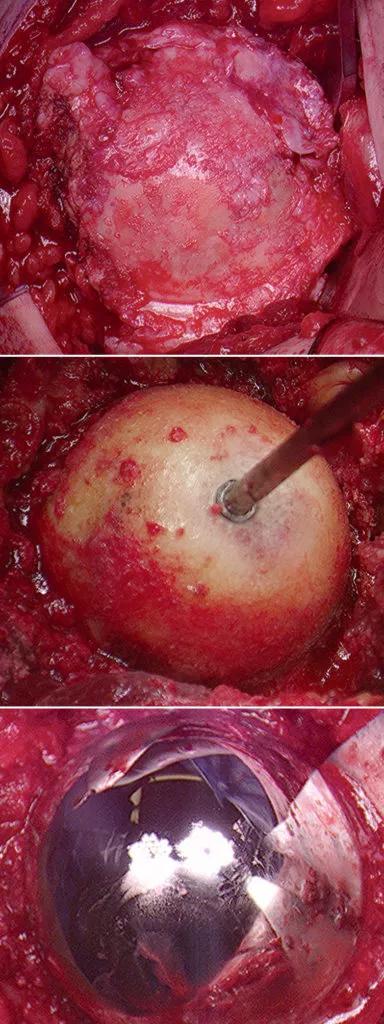
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b949e94c-e3dc-480f-8c7e-b5a81d5713f5/19-ORT-1452-Shoulder-CQD-Inset-1-384x1024_jpg)
Dr. Miniaci replaced the shoulder with a more anatomical procedure. The humeral head is replaced with a bone preserving oval implant which more closely replicated the patient’s anatomy.
Advertisement
Advertisement
How it’s similar but different from the direct anterior approach
Collaboration must cross borders and disciplines
Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols
Should surgeons forgo posterior and lateral approaches?
How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians
Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction
Percutaneous stabilization can increase mobility without disrupting cancer treatment