Recent data call for revisiting FDA surveillance recommendations
By Patrick Collier, MD, PhD; Muzna Hussain, MD; Zoran B. Popovic, MD, PhD; and Brian P. Griffin, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This article is reprinted from the February 2021 issue of the Cleveland Clinic Journal of Medicine (2021;88[2]:110-116).
Anti-human epidermal growth factor receptor 2 (anti-HER2) therapy has been a game changer for some forms of aggressive breast cancer, drastically reducing mortality rates. The FDA calls for close cardiac surveillance in patients receiving anti-HER2 drugs. But this recommendation is based on an early clinical trial with circumstances that often are no longer relevant. As it now stands, this strategy is burdensome, dangerous for patients who are unnecessarily advised to discontinue therapy and often ignored in practice.
This article discusses what drove the current FDA cardiac surveillance strategy for anti-HER2 therapy and the challenges it poses in practice and clinical research. Results of more recent clinical trials are reviewed and new best practices for anti-HER2 therapy management and cardiac monitoring are proposed.
About one in four patients with breast cancer has an aggressive tumor that overexpresses a tyrosine kinase receptor protein called human epidermal growth factor receptor 2 (HER2, also known as HER2/neu, CD340, Erbb2 and proto-oncogene Neu). It is encoded by the ERBB2 oncogene on chromosome 17.1 Signaling through this receptor promotes cell proliferation and opposes apoptosis; when it is overexpressed, uncontrolled cell growth results.
Patients with breast cancer undergo HER2 testing to assess prognosis and determine candidacy for personalized therapy. Over the past 20 years, agents targeted against HER2 have been developed, contributing to a halving of breast cancer mortality rates, in what is widely regarded as a phenomenal success story.2 Anti-HER2 agents include the following:3,4
Advertisement
Other targeted anti-HER2 therapies are continually being developed.
Current FDA recommendations regarding the frequency of surveillance of left ventricular function with anti-HER2 therapy are conservatively based on historical data involving patients receiving concomitant anthracycline therapy.5
The pivotal trastuzumab randomized controlled trial in patients with metastatic breast cancer, published in 2001, reported a 27% rate of cardiac dysfunction and a 16% rate of New York Heart Association (NYHA) class III or IV heart failure in patients who received trastuzumab with anthracycline chemotherapy.6 These findings prompted the FDA to issue a stern package-insert warning of cardiomyopathy for anti-HER2 treatments, as well as recommendations for cardiac surveillance.
Trastuzumab’s package insert recommends measuring left ventricular ejection fraction (LVEF) before starting therapy, every three months during treatment and at the completion of therapy. If drug therapy is withheld for cardiotoxicity, studies should be repeated monthly. Furthermore, after completion of therapy, LVEF should be measured every six months for at least two years.5 Thus, a minimum of nine echocardiograms is recommended for patients undergoing a standard 12-month adjuvant dosing schedule, with potentially lifelong continuation of echocardiographic assessment every three months for those with metastatic disease on continual anti-HER2 therapy.
Subsequent clinical trials7-16 have generally indicated a more favorable cardiac profile, as detailed in Table 1 (available here in the original Cleveland Clinic Journal of Medicine version of this article).
Advertisement
The 2007 Herceptin Adjuvant (HERA) trial found a 3% rate of cardiac dysfunction and a 0.6% rate of NYHA III or IV heart failure.17 A 2019 trial8 found that only 1.2% of patients discontinued dual therapy because of decreased ejection fraction, while adjudicated cardiac events occurred in less than 1%. The relationship between decreased ejection fraction assessed by cardiac monitoring and the development of clinical heart failure was not discussed.
Although the risk of cardiac dysfunction from anti-HER2 therapy now appears low, the FDA package-insert warning and recommendations remain. Extensive cardiac monitoring and echocardiographic testing regimens are still part of the standard protocols of clinical trials involving anti-HER2 therapy.8,11,18,19 In a 2017 trial,11 up to 13 imaging studies (preferably echocardiograms) were scheduled using the following protocol: at baseline, during treatment (at chemotherapy cycles 2, 6, 10 and 14) and during follow-up (months 3, 6, 12, 18, 24, 36, 48 and 60), resulting in a potential total of 19,318 studies for 1,486 patients.
Several factors may help explain different event rates between clinical trials of the same drug:
Advertisement
More than 50 years ago, Wilson24 wrote about the attributes of an ideal screening test and advised caution: “In theory, screening is admirable, but in practice there are snags; the central idea is simple and may appear deceptively straightforward.”
Wilson’s screening criteria and their applications to surveillance echocardiography during chemotherapy are presented in Table 2 (available here in the Cleveland Clinic Journal of Medicine version of this article).24
Currently, LVEF is the screening variable of choice.19 Strain assessment is a nonactionable supportive tool. However, it is the focus of ongoing research and is increasingly being used, especially as it received a formal CPT code from the Centers for Medicare & Medicaid Services.25
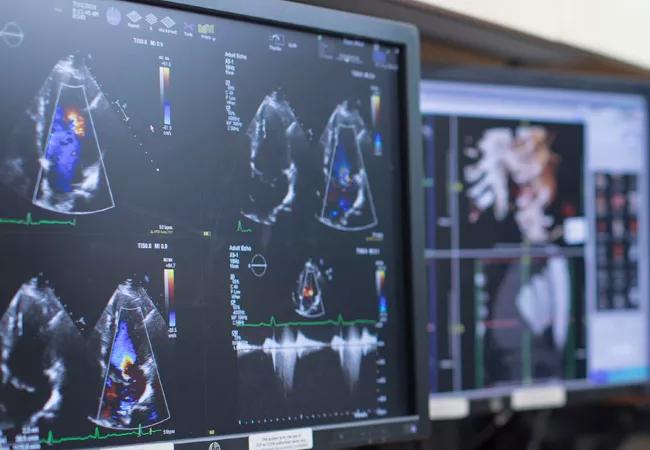
Echocardiography is the preferred screening method, although cardiac magnetic resonance imaging is considered to be the gold standard and is advised in selected cases (i.e., if echocardiographic images are inadequate or yield equivocal findings). Another option, multigated acquisition radionuclide scanning, is not a first-line test, as it involves radiation and introduces cross-modality error.
The net benefit of therapy refers to balancing the risks of toxicity with prognosis and available treatment options. Potential cardiotoxicity may be more acceptable in the setting of a cancer with a poor prognosis and few treatment possibilities. On the other hand, cardiotoxicity is less likely to be an acceptable risk for a later-generation drug in a cancer with multiple existing therapies and a generally good prognosis.
Advertisement
Regarding breast cancer, regimens without an anthracycline have been shown to be as effective as those with an anthracycline, especially for women at low risk of recurrence. Strategies without an anthracycline involve much lower rates of cardiotoxicity, with rates of NYHA class III and IV heart failure being close, if not equal, to those with placebo (0.4% over five years or fewer than 1 per 1,000 patients per year).18 They have also demonstrated improved survival and favorable cardiac safety for metastatic cancer.26
Because anti-HER2 treatment is used against a particularly aggressive cancer, decisions regarding interrupting or stopping it based on side effects have especially important implications. Whether such decisions should be made based on a surrogate echocardiographic endpoint, possibly in the absence of symptoms, needs careful consideration.
Anti-HER2 treatment in patients with preexisting cardiac dysfunction has been associated with a worse prognosis and higher rate of symptomatic heart failure compared with patients with preserved ejection fraction at baseline.27 However, preexisting cardiac dysfunction is a relative rather than an absolute contraindication to starting anti-HER2 treatment. The FDA recommends extreme caution in treating such patients,5 and a cardiologist should be involved in management.
For patients who develop clinically significant congestive heart failure, discontinuing anti-HER2 therapy should be strongly considered. For patients without symptoms, treatment-specific LVEF thresholds for stopping medications have been developed, with slightly different recommendations between FDA-approved labeling, clinical trial protocols and professional society guidelines. Criteria from clinical trials that do not involve anthracycline therapy tend to be a little less stringent because anti-HER2-associated toxicity is considered to be dose-independent, nonapoptotic and potentially reversible (type 2 cardiotoxicity). In contrast, anthracycline-mediated cardiotoxicity is regarded as type 1 (i.e., irreversible and related to cumulative dose).28
A commonly used threshold defining cardiotoxicity is a decrease in LVEF of more than 10% to a value below the lower limit of normal. Hussain et al,29 in a study of 23 patients with asymptomatic LVEF decline who continued trastuzumab, found that 14 patients (61%) tolerated it without a cardiac event, six (26%) developed further worsening of LVEF, one (4%) developed heart failure and two (9%) died of a possible or probable cardiovascular cause.
Strategies to prevent or attenuate cardiotoxicities include participation in cardio-oncology programs (particularly for symptomatic or high-risk patients being considered for anti-HER2 treatment, including anyone with baseline low LVEF), early recognition of cardiac side effects, active cardiac surveillance and cardioprotective medical therapy.
Accurate diagnosis of cardiotoxicity is critical, as false-positive results may lead to inappropriate stopping of potentially lifesaving chemotherapy.
Serial echocardiography in patients with cancer can be difficult, and measurement variability may be high. Reasons may be technical (e.g., concomitant lung disease, high or low body mass, postoperative status) or involve confounding factors (e.g., variable hemodynamics, medications, fluid status).30
Outside of trial settings, false-positive results are not infrequent. In addition, pre-chemotherapy studies may manifest hyperdynamic function. Teasing out whether serial changes are related to cancer therapy versus comorbid illness (e.g., concomitant arrhythmia, ischemia, stress cardiomyopathy, and myocarditis) may be challenging.
Optimizing measurement accuracy.Repeat echocardiographic studies should be performed in as consistent a manner as possible (e.g., same equipment, technician and reporting physician). Multiple ways to measure LVEF should be used, including quality 3D echocardiography (ideally without contrast for highest reproducibility), the biplane Simpson method (with contrast, if necessary) and visual assessment, with reporting of the best available data.19 Global longitudinal strain may provide corroborative data when concordant; if discordant, the quality of the data should be reviewed again with particular attention to wall tracking. Ideally, differences between serial tests should be compared to the maximal detectable difference, a value that can be calculated for each echocardiographic laboratory, providing a threshold to distinguish likely test error from real change.31 For borderline cases, obtaining an experienced second opinion, an early interval repeat study or an alternative test (e.g., cardiac magnetic resonance imaging) should be considered.
Treating chemotherapy-related cardiomyopathy remains a challenge.Applying current guideline-directed heart failure management to chemotherapy-related cardiomyopathy can be particularly challenging. Especially for patients undergoing chemotherapy, titrating levels of beta-blockers and renin-angiotensin system antagonists to optimal dosing is often difficult because of poor tolerability. Outside these guidelines, data to support the use of cardioprotective medical therapy to prevent chemotherapy-related cardiotoxicity are modest at best. Studies are limited by marginal effect size, small patient numbers and short follow-up.
Should general cardiotoxicity screening be eliminated?Many have questioned the usefulness of currently proposed cardiac monitoring for patients on anti-HER2 therapy, particularly for those who are asymptomatic, do not have cardiovascular risk factors and have not received concomitant anthracycline therapy.32 Data assessing the cost-effectiveness of screening strategies for cardiotoxicity are limited.33 To avoid placing additional financial and time burdens on patients with cancer and their families, some have suggested that simply monitoring patients on clinical parameters alone is best.26
Current practice regarding screening for chemotherapy-related cardiomyopathy is a legacy of its mutable historical background. It is overshadowed by variable and conflicting guidelines, with the result that most patients on anti-HER2 treatment actually receive minimal or no cardiac imaging.34,35 If oncologists are voting with their feet, it appears that recommendations are perceived as promoting overtesting, with a common result being minimal or no testing in actual practice.
We suggest a more focused cardiac surveillance approach to low-risk, asymptomatic patients receiving anti-HER2 treatment. Routine serial LVEF measurement by echocardiography should be done only if patients have received anthracyclines or are considered to be at high risk (e.g., concomitant hypertension, borderline low LVEF). For these patients, studies should be carried out at baseline, post-anthracycline (if appropriate) and every three months while on anti-HER2 treatment. Less-frequent testing may be justified for patients with metastatic disease who have repeatedly normal LVEF test results. Patients should be informed about potential symptoms of cardiotoxicity and advised to report them promptly.
Drs. Collier, Popovic and Griffin are all staff in Cleveland Clinic’s Department of Cardiovascular Medicine, with Dr. Collier also serving as Co-Director of the Cardio-Oncology Center and Dr. Griffin as Section Head, Cardiovascular Imaging. Dr. Hussain is a cardiovascular research fellow in the Department of Cardiovascular Medicine.
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more