An alternative to surgery when other therapies fail
By Ihab Haddadin, MD, and Gustavo Heresi, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 67-year-old woman had a history of hereditary spherocytosis for which she underwent splenectomy in 1975. She first developed a pulmonary embolism in 2012 after hip surgery and was treated with warfarin for one year. A year later she remained dyspneic and hypoxemic. A right heart catheterization showed mild precapillary pulmonary hypertension, for which she was started on oral tadalafil and ambrisentan. She continued to deteriorate, and in early 2017 was re-evaluated with a ventilation-perfusion (VQ) scan and CT chest scan, which were consistent with chronic thromboembolic disease. She was started on anticoagulation therapy and inhaled treprostinil, and her tadalafil was switched to riociguat.
Upon evaluation at Cleveland Clinic’s chronic thromboembolic pulmonary hypertension (CTEPH) program in 2018, the patient had NYHA Class III dyspnea, exertional desaturation and a six-minute walk distance of only 860 feet. Right heart catheterization showed severe precapillary pulmonary hypertension with a mean pulmonary artery pressure of 52 mmHg, cardiac output of 3.7 L/min and pulmonary vascular resistance of 11.6 Wood units — even though the patient was on three pulmonary vasodilators. Perfusion defects on VQ scan were segmental or smaller in the lingula, right middle and right lower lobes. CT chest and digital subtraction pulmonary angiography showed disease in proximal segments of the right lower lobe and medial segment of the right middle lobe, as well as disease in distal segmental and subsegmental vessels in the lingula and left lower lobe. There were areas of subpleural hypoperfusion distal to non-occluded vessels, consistent with small vessel disease.
Advertisement
Her case was deemed inoperable by our multidisciplinary CTEPH group due to the discrepancy between the degree of pulmonary vascular resistance elevation and the thrombotic burden (suggesting prominent microscopic vasculopathy), distal segmental and subsegmental disease on the left, and history of splenectomy, which is associated with poorer response to surgery due to concomitant microvascular disease.
Careful anatomic assessment was performed using advanced imaging techniques, including cone-beam CT and optimal coherence tomography.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c2b60932-1013-446b-a343-33cbdcf65339/18-PUL-4960-Heresi-Figure-02-650pxl-width_jpg)
Cone-beam CT indicates narrowing and possible webbing after the initial recanalization and angioplasty.
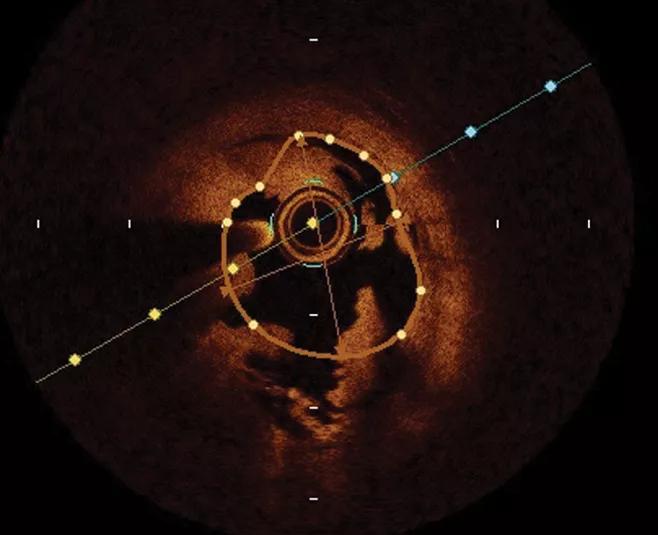
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eca37ba3-4724-42f4-b612-5a1f4f265e53/18-PUL-4960-Heresi-Figure-03-650pxl-width_jpg)
Optical coherence tomography clearly delineates the pathology of webbing associated with chronic thromboembolic pulmonary hypertension.
The patient underwent six balloon pulmonary angioplasty (BPA) sessions, treating several segments in the right lower, middle and upper lobes.
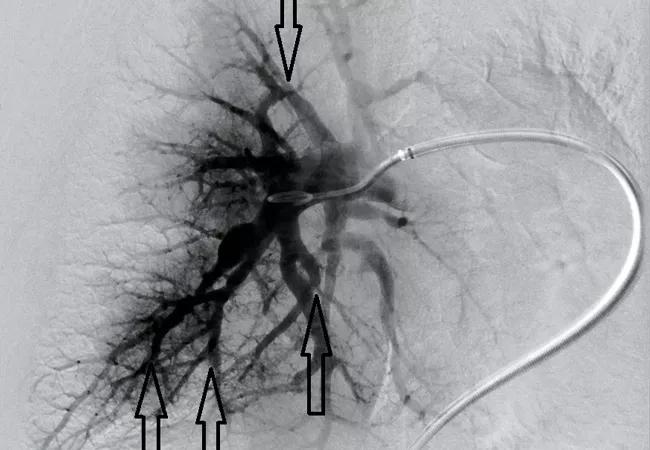
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/382289b4-ae3b-49a0-af13-663af79dfef0/18-PUL-4960-Heresi-Hero-Image-650x450pxl_jpg)
The angiographic appearance after balloon pulmonary angioplasty shows dramatic improvement in blood flow.
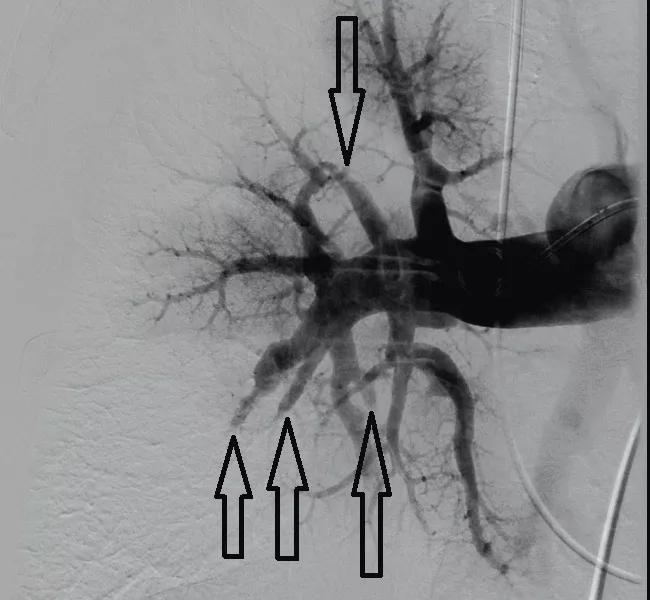
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/444d7b6a-3171-4c36-8a9a-9977a9acc295/18-PUL-4960-Heresi-Figure-04-650pxl-width_jpg)
The angiographic appearance of the right lower lobes before balloon pulmonary angioplasty shows poor blood flow.
The patient improved dramatically. She now has NYHA Class II symptoms. She no longer desaturates with activity. Echocardiography shows significant decrease in tricuspid regurgitation. Right heart catheterization shows significant improvement in hemodynamics, with a mean pulmonary artery pressure of 32 mmHg, cardiac output of 5.1 L/min and pulmonary vascular resistance of 5.5 Wood units. She is scheduled to undergo further BPA sessions to treat the left lung.
Advertisement
Cleveland Clinic offers BPA as an excellent treatment option for select patients with inoperable CTEPH.
Dr. Heresi is Medical Director of the Pulmonary Thromboendarterectomy Program in the departments of Pulmonary and Critical Care Medicine at Cleveland Clinic.
Advertisement
Advertisement

Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program