Devastating long-term effects in a young adult patient
A 26-year-old female presented to the emergency department with polydipsia, polyuria and random glucose of 700 mg/dL. Her hemoglobin A1C was 7.5%, and she was diagnosed with diabetes. A bone densitometry test showed a Z score of -1.7 in the spine, less than expected for age.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
She had previously been diagnosed with autoimmune hepatitis and required high doses of intravenous steroids, azathioprine and tacrolimus. She also required a prolonged course of oral steroids. She eventually developed profound proteinuria and underwent a renal biopsy which showed membranous glomerulonephritis. Immunofluorescence showed a full house pattern. She had been referred to rheumatology, where her labs revealed high titer antinuclear antibodies, positive anti-Smith antibodies, normal anti-double stranded DNA antibodies, normal C3 and C4 and a normal complete blood count. She was later was diagnosed with systemic lupus with renal involvement and placed back on steroids with the addition of hydroxychloroquine.
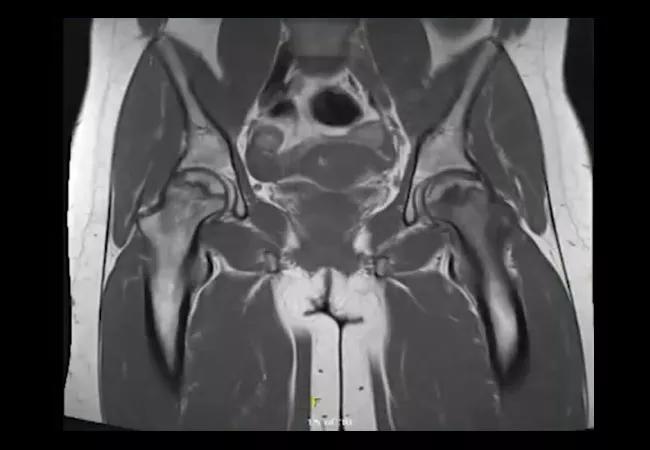
In the emergency department, her hemoglobin A1C was 7.5%, and she was diagnosed with diabetes. A bone densitometry test showed a Z -score of -1.7 in the spine which is less than expected for age. At follow up, she presented with bilateral groin and hip pain, but X-rays did not show obvious avascular necrosis. Bilateral magnetic resonance imaging of the hips showed left-sided acute-on-chronic avascular necrosis and chronic avascular necrosis of the right femoral head with a right-sided joint effusion. She eventually required bilateral hip replacements. Watch as Emily Littlejohn, DO, MPH, staff in the Department of Rheumatologic and Immunologic Diseases, discusses the case.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/u1A4dFF66Rw?feature=oembed)
A Patient With Steroid Toxicity
“The issues highlighted by this case include the devastating long-term effects of steroids, including steroid-induced diabetes, bone density less than expected for age and osteonecrosis of the femoral heads,” says Dr. Littlejohn. “We need to be aware of the modifiable risks of steroid toxicity.”
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis