A complex, acute disease diagnosis highlights the need for multidisciplinary management
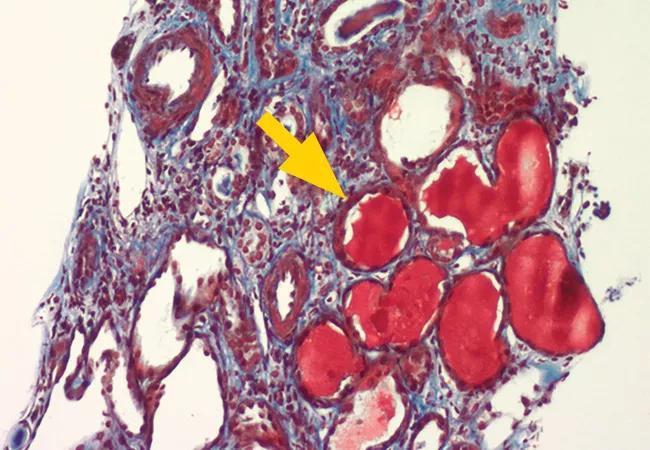
Above: A Jones stain demonstrates a view of a glomerulus with a suggestive collapsing lesion.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By Saja Almaaitah, MD, Jonathan Myles, MD, and Emily Littlejohn, DO, MPH
A 43-year-old female presented to Cleveland Clinic with acute-onset progressive fatigue, generalized weakness and bilateral lower-extremity swelling that had been going on for one month. On admission, she was found to have elevated systolic blood pressure (160/84 mmHg) and severe acute kidney injury with creatinine of 5.5 mg/dL, from a baseline of 0.7 mg/dL tested one year earlier.
A urine analysis revealed the presence of large blood and large protein. The patient’s urine protein creatinine ratio was significantly elevated at 9.9. An autoimmune workup was positive for antinuclear antibodies in addition to positive anti-Smith antibodies, anti-chromatin antibodies, anti-double-stranded DNA antibodies and cytoplasmic perinuclear antibody (p-ANCA). Nephrology and rheumatology teams were consulted and recommended a kidney biopsy that showed mild immune-complex mediated mesangiopathic glomerulonephritis with immunofluorescence staining positive for IgG, IgM, C3 and C1q, in addition to diffuse effacement of epithelial foot processes with possible collapse and segmental scarring, consistent with class II lupus nephritis with podocytopathy and collapsing glomerulosclerosis.
Lupus nephritis is one of the most common organ-threatening manifestations of systemic lupus erythematosus, occurring in up to 50% of patients with lupus, with 50% of those diagnosed progressing to end-stage renal disease.
Histology of lupus nephritis is characterized by mesangial, subendothelial and subepithelial immune-complex deposition on renal biopsy. Lupus podocytopathy is a rare manifestation of lupus kidney disease occurring in up to 2% of lupus nephropathy, and is characterized by diffuse epithelial cell foot process effacement, resembling histologic findings of minimal change disease or focal segmental glomerulosclerosis (FSGS). Collapsing glomerulopathy describes severe injury to podocytes with loss of markers of differentiation, proliferation of podocytes and global or segmental collapse of the glomerular capillary tuft. Lupus podocytopathy tends to be steroid responsive, though FSGS and collapsing subtypes are generally resistant to treatment and usually require aggressive immune suppression.
Advertisement
Given unusual findings of lupus podocytopathy and collapsing glomerulosclerosis, the biopsy results and treatment options were thoroughly discussed with the pathology, nephrology and rheumatology teams. The patient received intravenous (IV) pulse dose methylprednisolone of 1 g daily for three days and was started on IV cyclophosphamide 500 mg every two weeks for a total of six doses (EURO lupus protocol). Creatinine increased during hospitalization to a peak of 6.32 mg/dL and started to decline soon after the initiation of treatment. This was associated with improved lower limb swelling and energy level.
A good urine output was maintained throughout the patient’s disease course. In addition to the cyclophosphamide protocol, the patient was discharged from the hospital on 60 mg daily of prednisone as part of a taper regimen. She was also started on hydroxychloroquine, pneumocystis prophylaxis and diuretics.
The patient completed induction therapy with cyclophosphamide infusions over three months. She was subsequently started on mycophenolate mofetil 1,000 mg PO twice daily. Her creatinine level returned to normal range (0.84 mg/dL). Proteinuria significantly improved, though persisted, with a urine protein creatinine ratio of 2.4.
Throughout patient’s entire clinical presentation, she never developed other manifestations of lupus, including inflammatory joint pain, mucocutaneous ulcerations, rashes, alopecia or pleuritis. The patient is maintained on mycophenolate mofetil 1,000 mg twice daily, hydroxychloroquine 400 mg daily and prednisone 5 mg daily and continues to do well.
Advertisement
The complexity and acuity of this patient’s disease highlights the need for multidisciplinary management when caring for patients with systemic lupus erythematosus.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis