Concurrent treatment necessary for addressing progressive disease and infection
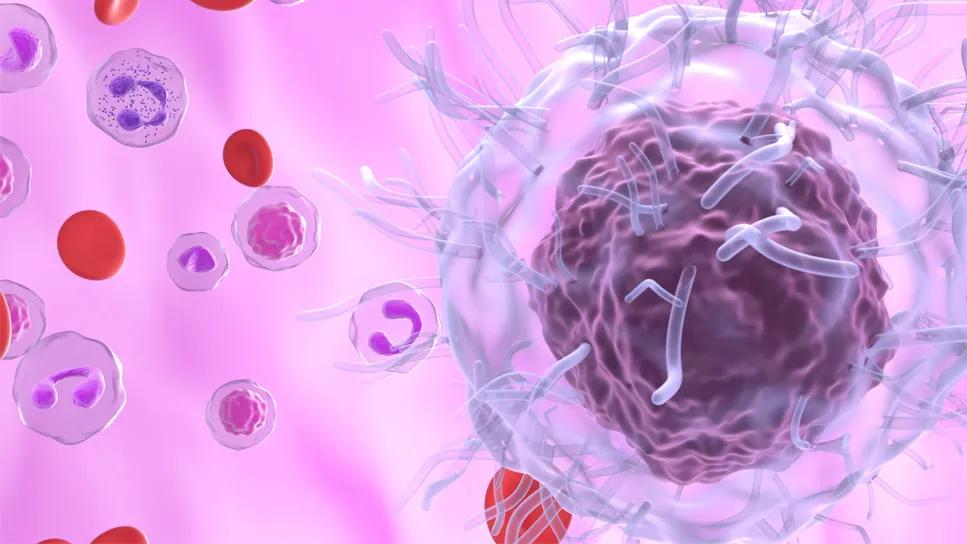
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c7788a60-e6ab-441a-89c3-90ba9f278eff/hairy-cell-leukemia-1635266531)
Hairy cell leukemia
After weeks suffering from unexplained fevers and night sweats, a 53-year-old Caucasian man was transferred from an outside hospital to Cleveland Clinic to identify the underlying cause of his symptoms. After a multifaceted workup, the care team diagnosed the patient with hairy cell leukemia. Complicating the picture was a bloodstream infection with methicillin-sensitive staphylocuccus aureus, which had spread to infect the valves of his heart. Rapid intervention and simultaneous treatments were needed to bring both conditions under control.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As a firefighter and EMT, the patient had been relatively healthy aside from having high blood pressure, diabetes and low back pain. He arrived at Cleveland Clinic quite ill. His right ankle was fractured and CT scans showed evidence of breakdown of the bone. He was also found to have severely decreased blood counts.
The Infectious Disease and Hematology teams conducted a thorough evaluation, analyzing his low blood counts and ordering a battery of blood tests and a bone marrow biopsy. At the same time, they provided supportive care for his severe immune suppression.
Initial tests found the patient had a bloodstream infection, with some of those bacteria infecting the ankle joint of his right foot, which required surgery to manage. “With this diagnosis, the inpatient team acted swiftly to identify one of the most feared consequences of bloodstream infection, which is an infection of the heart and heart valves,” explained Taylor Brooks, MD, a hematologist/oncologist with Cleveland Clinic. “We reached out to the Cardiac Surgery team and get them involved right away.”
Within days, the patient had an advanced echocardiogram, which confirmed a heart infection. Around the same time, the bone marrow biopsy revealed that the patient also had hairy cell leukemia, a rare disease that involves accumulation of abnormal B lymphocytes.
The severity of the illness meant the patient needed swift intervention on multiple fronts to bring the blood infection and leukemia under control. He received coordinated care across multiple specialties, including:
• Hematology to treat the leukemia
• Cardiothoracic surgery to repair his mitral valve
• Orthopedics to address hardware in his ankle that had become infected
While diagnosis of the blood infection was underway, the care team was deciding on the type and timing of surgery. At the same time, the patient began his cancer treatment.
Usually, standard first-line treatment for this type of leukemia involves chemotherapy, but this would have been potentially life-threatening, given his active infection and immunocompromised condition. Instead, the team chose to administer the oral medication vemurafenib, which is usually reserved for relapsed disease. “The rapid onset of this targeted medicine and favorable safety profile allowed us to control the disease while minimizing additional risks,” Dr. Brooks says.
A week after hospital admission, the patient underwent orthopedic surgery to remove the infected ankle hardware. After recovery from the orthopedic surgery and several weeks of receiving antibiotics and vemurafenib, the patient underwent open heart surgery.
During the procedure, Shinya Unai, MD, excised the infected area of the valve, repaired a defect in the valve and used prosthetic material to patch the area. After recovery, the patient was able to go home, where he continued a course of antibiotics as well as the vemurafenib.
Roughly five months later, the patient underwent a second open heart surgery to complete the repair of the infected heart valve. After his recovery from surgery, he was well enough to transition from vemurafenib to a combination of rituximab and cladribine, which are the standard of care for treating hairy cell leukemia.
“This case highlights the importance of performing steps in parallel when time is of the essence,” says Dr. Brooks.
Advertisement
The interventions were successful and the patient made a full recovery. He achieved a complete remission from leukemia and the blood infection cleared. His blood counts also returned to normal.
The patient’s care team reported that he is feeling well and has returned to work part time.
The compound nature of this case required a special approach. Dr. Brooks shared several takeaways from treating this patient:
• Diagnosis of rare cancers requires pathologists who see a volume of these types of cases. “Rare disease diagnosis is challenging. Missed diagnosis or misdiagnosis can occur if pathology doesn’t have the expertise in uncommon cases. We’re very fortunate to have hematopathologists with a great deal of experience in this realm,” says Dr. Brooks.
• Tailor therapy to the individual patient. In this case, deviating from the standard therapy allowed the patient’s immune function to be restored enough to fight the infection and for him to then transition to a more robust anti-leukemia therapy once he was healthy enough.
• Engage multidisciplinary care. “We could not have properly cared for the patient if it weren’t for multiple specialties working together to provide timely and essential care,” says Dr. Brooks. “Direct interaction between Hematology and Cardiac Surgery was an important aspect of the patient’s infection care.”
• Break care into stages. For this patient, the team developed a framework for the patient’s initial stabilization, recovery and definitive treatment care phases, bridging inpatient and outpatient care. “This approach requires expertise, discerning judgment as well as the infrastructure to ensure that coordination and transitions happen safely and effectively,” says Dr. Brooks.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches