How to time the interventions, and how to manage anesthesia risks?
In mid-2021, a 55-year-old man with advanced idiopathic pulmonary fibrosis came to Cleveland Clinic from another state to be evaluated for lung transplantation. He was evaluated by transplant pulmonologist Shruti Gadre, MD, who noted that his clinical status had progressively declined for several months and his need for supplemental oxygen had significantly increased. Dr. Gadre admitted him to the transplant service for expeditious evaluation and consideration for urgent transplantation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During exhaustive pre-transplant evaluation, a previously known but stable large (6.2-cm) abdominal aortic aneurysm was brought to light. “Even if the patient had not known about the aneurysm, abdominal imaging done as a part of the transplant evaluation would have revealed it,” says Dr. Gadre, noting that the evaluation includes thorough examination of all organ systems to identify any additional life-threatening issue that could undermine the benefit from transplantation.
An abdominal aortic aneurysm of this size requires intervention, as it carries a significant risk of rupture and a 10% to 20% mortality risk per year. This risk can be exacerbated by hemodynamic variations that are common during major surgeries, including lung transplant. The aneurysm complicated the decision to proceed with transplantation, so Dr. Gadre discussed management options with thoracic surgeon Usman Ahmad, MD, and vascular surgeon Francis Caputo, MD.
In the setting of advanced pulmonary fibrosis, a major elective surgery such as aortic aneurysm repair carries significant risk of respiratory failure and death from perioperative complications. “We felt that general anesthesia would be prohibitive, given the risk of long-term intubation and the potential for complications prior to transplant,” Dr. Gadre explains.
In response, Dr. Caputo was able to plan an endovascular aneurysm repair (EVAR) that could be performed without general anesthesia, using only light sedation and local analgesia. Additionally, multiple teams came together to clarify the patient’s candidacy for lung transplant in case he developed respiratory failure.
Advertisement
After further discussion among members of the vascular service, thoracic service and lung transplant team, it was determined that the patient could and should undergo EVAR prior to transplantation. The plan was approved by Cleveland Clinic’s multidisciplinary transplant selection committee.
A vascular surgery team led by Dr. Caputo successfully stented the patient’s 6.2-cm aneurysm using only light sedation with lidocaine at the puncture site. The patient experienced no complications from the 90-minute EVAR procedure. Figure 1 presents images of the aneurysm before and after intervention.
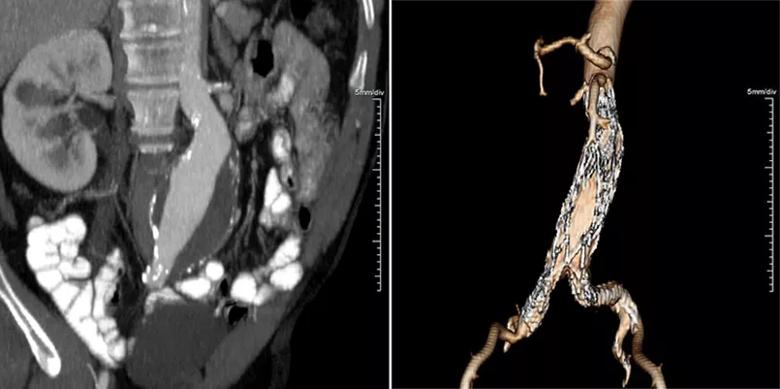
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f9131973-0ceb-4b8a-a0aa-06dd35ab9f77/21-HVI-2595510-Figure-1-1_jpg)
Figure 1. A preoperative CT of the patient’s aneurysm (left) in contrast to a 3D reconstruction image (right) taken three months after EVAR showing complete exclusion of the aneurysm.
Two days after EVAR, the patient was placed on the transplant list, at which time a careful anesthetic and operative plan was developed under the umbrellas of Cleveland Clinic’s Heart, Vascular & Thoracic Institute and Respiratory Institute.
Three days after listing, the patient received two new lungs in a successful transplant performed by cardiothoracic surgeon Shinya Unai, MD. He was discharged home two weeks later, breathing room air, and has had an uneventful recovery. Figure 2 presents chest X-rays before and after transplant.
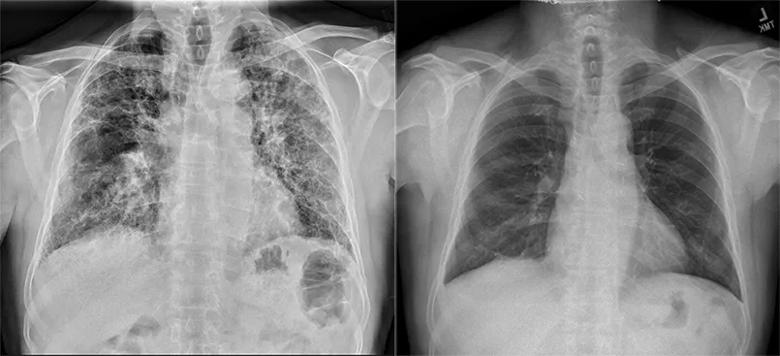
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9ecc2faa-9f50-4661-8576-61b7f4797917/21-HVI-2595510-Figure-2_jpg)
Figure 2. Chest radiographs of the patient before (left) and after (right) double lung transplant. Note the severe idiopathic pulmonary fibrosis in the pre-transplant image.
Treatment of two life-threatening diseases requires a multidisciplinary team of motivated physicians and surgeons to guarantee the best possible outcome.
Advertisement
“The true essence of teamwork, and the value of collaborative multidisciplinary care by high-performance teams, is highlighted by cases like this with multiple high-risk scenarios,” says Dr. Ahmad, the thoracic surgeon involved in the patient’s evaluation. “These are the opportunities that allow us to come together routinely to provide high-end world-class care.”
“This case underscores the importance of thorough transplant screening and identifying the right experts to collaborate to deliver precisely the care that patients need,” Dr. Gadre adds. “There was a broad commitment to doing whatever was necessary to safely address both of this patient’s serious conditions in the order that optimized the chances of a good outcome. Thanks to his experience, Dr. Caputo didn’t hesitate to operate on a patient who was in the medical ICU on a high-flow oxygen system requiring a fraction of inspired oxygen of 50%.”
“Success in complex cases like this demands good interdisciplinary communication,” Dr. Caputo observes. “We talk with each other and try to come up with the best plan. Sometimes patients with the most complex cases can feel like they’re on a remote island. It’s hard to be on an island, but when there’s a wide-ranging group of experts on the island with you, creative solutions can be found.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center