Matching the minimally invasive CABG alternative to the right candidates
In August 2020, a 62-year-old male triathlete arranged a virtual visit with clinical cardiologist Tamanna Singh, MD, Co-Director of Cleveland Clinic’s Sports Cardiology Center. After hearing Dr. Singh on a recent podcast on heart health and running, he became concerned that his recent jaw pain and decline in stamina might be atypical symptoms of heart disease. Based on the virtual visit, Dr. Singh recommended that he have a cardiac catheterization done locally. When it revealed a severely diseased left anterior descending artery (LAD) and diseased circumflex artery, he came to Cleveland Clinic for an in-person evaluation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Because the patient had a history of pericarditis, Dr. Singh ordered a cardiac MRI to rule out active inflammation or constriction effect on the heart; she also ordered a repeat catheterization to confirm the location and extent of his coronary artery disease. The catheterization, performed by interventional cardiologist Jaikirshan Khatri, MD, included pressure-wire interrogation of the circumflex. When this was negative, Dr. Khatri confirmed that the patient’s disease was confined to the LAD.
Since revascularization via coronary artery bypass grafting or stenting would be necessary, Drs. Singh and Khatri met with cardiothoracic surgeon Faisal Bakaeen, MD, to discuss treatment options. A significant intramyocardial segment of LAD identified by Dr. Khatri on catheterization made stenting unwise. Dr. Bakaeen felt the patient would be an excellent candidate for minimally invasive direct coronary artery bypass (MIDCAB) grafting and would derive greater benefit from bypass grafting than stenting, owing to his age and activity level and the large myocardial territory he had at risk. The patient agreed to proceed with MIDCAB so long as all attempts would be made to avoid sternotomy.
The patient was anesthetized and prepared for off-pump surgery. Dr. Bakaeen made a small left thoracotomy incision, harvested the internal thoracic artery (ITA) and connected it to the LAD distal to the obstruction.
Graft flow was measured with a flowmeter and found to be ideal. After heparin was reversed, graft flow was rechecked and continued to be excellent. The wound was closed, and the patient was sent to the ICU. Two days later, graft patency was confirmed by coronary CT angiogram. The patient’s recovery was uneventful, and he was discharged home on postoperative day three. He is pleased with the limited extent of his scar (Figure 1).
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/07f28795-0107-4e7f-8937-3c67b3bb4418/Cropped-incision-photo_jpg)
Figure 1. Photo of the patient’s postoperative scar.
Although single-vessel disease is often treated medically or with stenting, MIDCAB offers many advantages for appropriately selected patients with suitable anatomy.
In this patient, borderline findings of disease in the circumflex artery seen on the first angiogram were ruled out with a second catheterization and pressure-wire interrogation. Concerns about potential constriction due to pericarditis were eliminated with an MRI.
Although the patient was leaning toward stenting to avoid a sternotomy, the team explained that because a segment of his LAD was buried in the myocardium, a stent would not be optimal due to a risk of continued symptoms and an increased risk of sudden cardiac death.
MIDCAB would be a better option, they noted, since an ITA graft to the LAD is likely to stay open in perpetuity.
In addition to being durable, MIDCAB offers advantages over traditional on-pump coronary artery bypass grafting, such as less scarring, shorter length of stay, less pain and quicker recovery. Because the operation is typically done off pump, patients experience less bleeding and potentially fewer complications and have lower risk of atrial fibrillation and stroke.
With a sternotomy, strenuous activity and heavy lifting are restricted for six to eight weeks as the sternum heals. With MIDCAB, those restrictions are loosened and governed by pain levels.
“Patients can gradually increase their activity,” says Dr. Bakaeen. “Once they feel no pain, they can generally perform most activities with few limitations.”
Advertisement
A key initial consideration for MIDCAB candidacy is making absolutely certain the patient has single-vessel LAD disease, says Dr. Khatri. “MIDCAB is not technically feasible if the patient has multivessel disease,” he explains. Other important considerations are the patient’s chest anatomy and the location and quality of the LAD target.
In addition to careful patient selection and input from a multidisciplinary heart team, successful MIDCAB requires quality control. At Cleveland Clinic, this is done by measuring graft flow in the operating room and often verifying graft patency with CT coronary angiography prior to discharge (Figure 2).
“This gives us a look at graft functionality and anatomy and provides confidence the graft is working well,” Dr. Bakaeen explains.
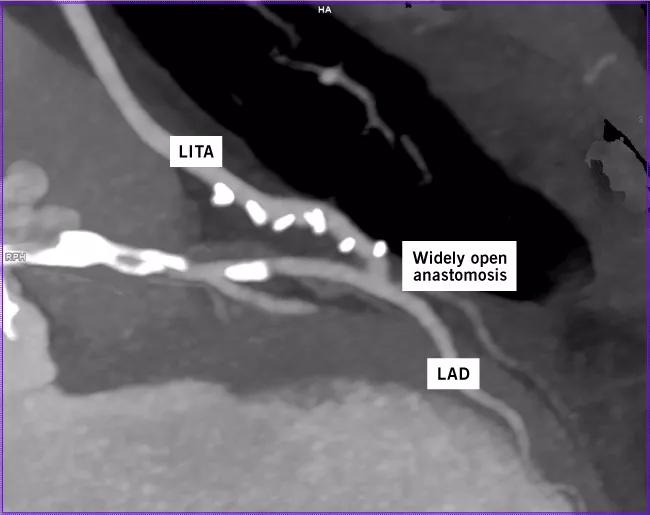
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/468f571f-99a3-4937-b929-484e40f32ba3/20-HVI-2029540_Bypass5_Label_jpg)
Figure 2. CT coronary angiogram showing a patent left ITA (LITA) with clips on its branches (bright white) anastomosed to the LAD beyond the diseased and calcified segments (also bright white).
As with other minimally invasive procedures, MIDCAB cannot always be guaranteed. Sometimes the patient’s anatomy or condition prevents carrying out the approach as planned. When this occurs, the surgeon makes adaptations to ensure the patient has the best outcome.
“We always start with a very small incision between the ribs,” says Dr. Bakaeen, “but if the LAD cannot be adequately exposed or if other factors preclude a safe or effective MIDCAB approach, then we have no hesitation to convert to sternotomy with or without use of a heart-lung machine. We never compromise safety or outcomes.”
Advertisement
In this case, the MIDCAB went as planned. “MIDCAB was a fantastic option for this patient, and he was very happy with the outcome,” concludes Dr. Singh.
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon
How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR
Optimal management requires an experienced center