Nasal bridge inflammation, ear swelling and neck stiffness narrow the differential diagnosis
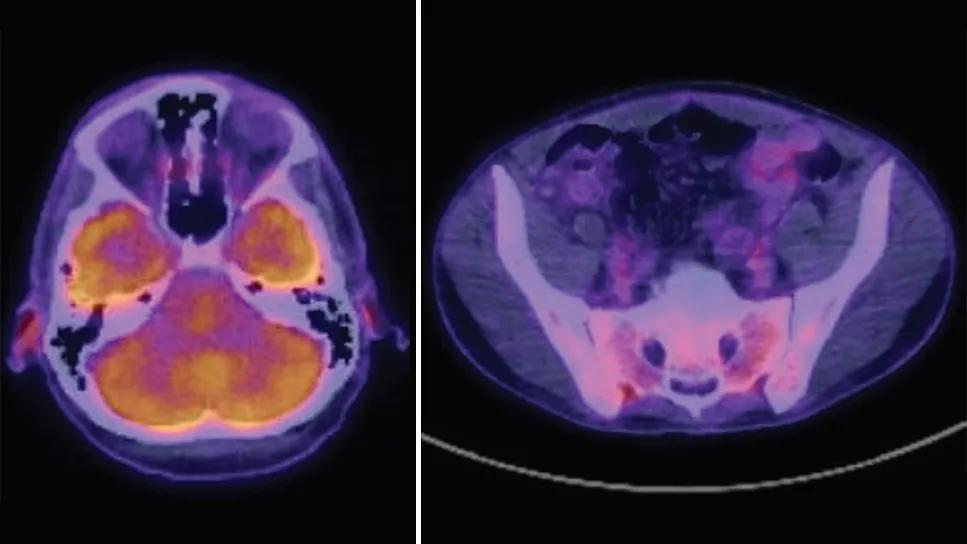
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c03f71b5-50a8-4f82-b0ce-754ab0828cf2/relapsing-polychondritis-imaging)
scan images of auditory canal and sacroiliac joints
By Adam Brown, MD, Ahmed Abuyakoub, MD, and Matthew Mandell, DO
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Background
A 41-year-old Caucasian male with a history of asthma and gastroesophageal reflux disease presented with generalized body pain, neck pain, shortness of breath, episodic chest pain, articular and nasal pain, and unintentional weight loss for one year. Because of the weight loss and concern for malignancy, a chest CT was performed, revealing right-greater-than-left perihilar lymph nodes as well as chronic calcification of the tracheal rings. A bronchoscopy with bronchial alveolar lavage was negative for infection, and ultrasound-guided biopsy of hilar adenopathy revealed reactive changes.
Additional imaging of the patient's abdomen revealed para-aortic retroperitoneal lymph nodes. The patient was transferred to Cleveland Clinic for consideration of an additional tissue biopsy. A positron emission tomography (PET) scan demonstrated patchy increased metabolic uptake in the cervical spine along with the bilateral sacroiliac (SI) joints, anterior costovertebral joints, and external auditory canal cartilaginous segments (see images above).
The unusual pattern of PET scan uptake with axial involvement raised questions about underlying spondyloarthritis, and Rheumatology was consulted. At this point, the patient was still feeling generalized weakness along with pain, primarily in his neck. During a rheumatologic evaluation, the patient also noted nasal and auricular pain. On exam he had saddle nose deformity and erythema with swelling of the right ear, and pain to palpation of both. His neck had a limited range of motion. He did not have appreciable synovitis on his extremities. His muscle strength was normal in the upper and lower extremities. His lab work was notable for an elevated white blood cell count and elevated inflammatory markers. Autoimmune serologies, including ANCA, and syphilis testing were negative.
Advertisement
With the weight loss, weakness, lymphadenopathy and elevated inflammatory markers, the initial concern about underling malignancy was understandable. He also had clear nasal and auricular chondritis as well as imaging (PET and MRI) evidence of axial inflammatory arthritis. The previous chest images also revealed evidence of calcifications of the trachea, which can be seen in relapsing polychondritis (RP). Considering the unremarkable lymph node biopsy, the most likely diagnosis was thought to be RP with axial involvement (cervical and SI joints).
The patient was started on IV methylprednisolone 125 mg for three days, followed by 60 mg prednisone daily, along with methotrexate 15 mg daily and one dose of infliximab 7.5 mg/kg. He rapidly responded to immunosuppressive therapy with resolution of pain and improvement in inflammatory markers and was discharged home with a steroid taper.
A neck CT showed small, non-enhancing fluid collection/effusion in the retropharyngeal space spanning from approximately the C2 vertebral body level through the inferior aspect of C4.
This patient’s unusual pattern of disease and striking imaging findings are a reminder of the many ways relapsing polychondritis can present. The patient presented with rather nonspecific symptoms — fatigue, unintentional weight loss and joint pain. Although the initial concern was for underlying malignancy, the nasal bridge inflammation, ear swelling and neck stiffness turned the differential diagnosis to potential RP. The differential diagnosis for nasal bridge inflammation and auricular swelling is relatively narrow, most commonly RP, granulomatosis with polyangiitis (GPA), or syphilis, although the latter two were less likely in the context of negative serologies.
Advertisement
Auricular chondritis is the most common and characteristic manifestation of RP, noted in 85% to 95% of patients, with nasal chondritis only slightly lower at 60% to 75% of patients.1 Respiratory chondritis occurs in 30% to 60% of patients, involves either the upper or lower airway, and can be difficult to distinguish from the subglottic stenosis seen in GPA. GPA is typically localized in the subglottic airway and is circumferential, whereas RP is more tracheal and often more localized anteriorly with calcifications, which this patient had.
Some aspects of his presentation, however, are unusual. On physical exam, the patient had limited ability to rotate his neck, and the MRI demonstrated an edema-like signal change along the anterior longitudinal aspect of the upper cervical spine. The patient also complained of years of low back pain and evidenced sacroiliac pain with palpation. A pelvic MRI showed edema-like changes surrounding the SI joints, predominantly in the posterior ligamentous portion, rather than inflammation in the joints themselves, which is typically seen in spondyloarthritis. There were similar edema changes in the paravertebral muscles and ligaments at multiple levels. Axial involvement in RP is a rare manifestation.
Reassuringly, the patient responded rapidly to glucocorticoids and tumor necrosis factor (TNF) inhibition and was able to be discharged. Upon follow-up, his glucocorticoids were tapered to nearly zero. He was tolerating TNF inhibition, his pain had diminished, and his range of motion had substantially improved.
Advertisement
Advertisement
Advertisement
Unraveling the TNFA receptor 2/dendritic cell axis
Genetic testing at Cleveland Clinic provided patient with an updated diagnosis
From dryness to diagnosis
Multiple comorbidities are associated with pediatric psoriasis
Untreated seropositive erosive RA led to peripheral ulcerative keratitis
New clinic meets Hispanic patients where they are
Treatment strategies require understanding of pathomechanisms
Multidisciplinary care for patients with immune-related adverse events