Untreated seropositive erosive RA led to peripheral ulcerative keratitis
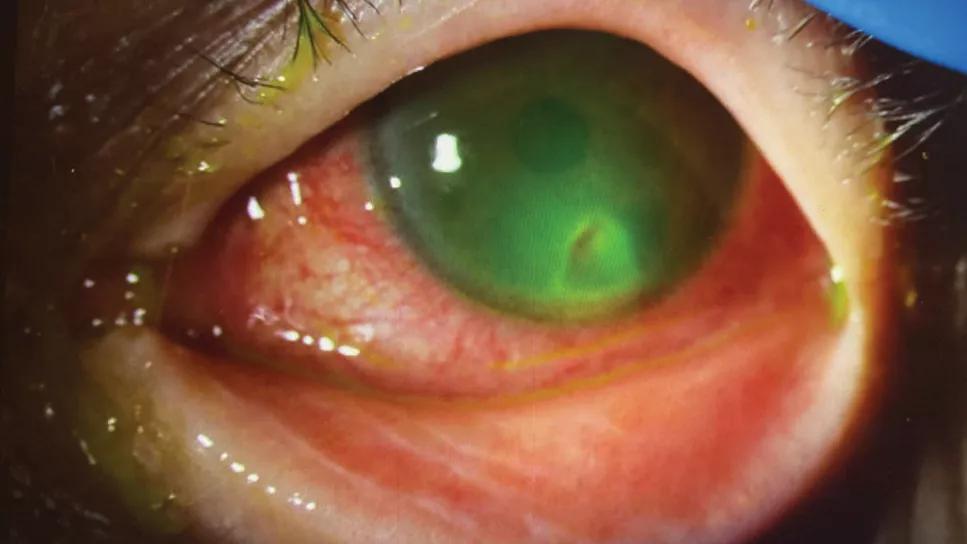
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4d4d9b5b-c632-4139-911a-8d72109f4a1d/peripheral-ulcerative-keratitis)
Closeup of eye with peripheral ulcerative keratitis.
By Taylor Koenig, MD, and Kinanah Yaseen, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An 81-year-old female presented to Ophthalmology with a monthlong history of left-eye blurry vision, foreign body sensation, irritation and photophobia. Her ophthalmologic examination revealed peripheral ulcerative keratitis (PUK) with scleritis of her left eye, which was confirmed on slit-lamp examination with fluorescein staining (above).
Bacterial culture of corneal scrapings was negative. She was started on oral glucocorticoid therapy out of concern for underlying autoimmune etiology of her inflammatory eye disease.
The patient reported that she had been diagnosed with rheumatoid arthritis (RA) 20 years before and was treated with intermittent non-steroid anti-inflammatory medications. She had never been treated with a disease-modifying agent or biologic therapy and had not followed
up with a rheumatologist since this diagnosis.
The patient was referred to Rheumatology, where her evaluation was
significant for ulnar deviation of her hands, positive rheumatoid factor of 24 IU/mL (normal range <16 IU/mL), and bilateral hand/wrist radiographs with metacarpal and intercarpal joint space narrowing and erosions.
The patient’s peripheral ulcerative keratitis was determined to be an extra-articular manifestation of her long-standing untreated seropositive erosive rheumatoid arthritis. Because of the severity of her disease, she was started on methotrexate and an anti-TNFα inhibitor for long-term treatment. Glucocorticoid therapy had not improved her significant ocular disease and was tapered. Eventually, rituximab was effective in controlling her arthritis as well as PUK.
Advertisement
RA is a chronic autoimmune disease that mostly affects the joints. Extra-articular organ involvement, including ocular and pulmonary manifestations, are common. They can be challenging to manage and associated with increased morbidity and mortality.
Ocular manifestations include sicca symptoms, episcleritis/scleritis and cornea melt, including PUK. Inflammation causes breakdown of collagen and stromal lysis of juxtalimbal cornea, which may lead to corneal perforation.
The underlying cause of PUK could be systemic, including infection or non-infectious causes such as RA, granulomatosis with polyangiitis and systemic lupus erythematosus. In RA, PUK can be unilateral or bilateral.
Clinical symptoms include redness, ocular pain, tearing and photophobia.
With the introduction of biologic therapy, the incidence and morbidity associated with PUK have reduced significantly. Rituximab has shown to be an effective treatment of RA-related PUK. At Cleveland Clinic, we work closely with Ophthalmology and other specialties in diagnosing and managing challenging rheumatic cases.
Advertisement
Advertisement
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma
Unraveling the TNFA receptor 2/dendritic cell axis
Nasal bridge inflammation, ear swelling and neck stiffness narrow the differential diagnosis
Genetic testing at Cleveland Clinic provided patient with an updated diagnosis
Study reveals more about the pathophysiology of Salzmann’s nodular degeneration
From dryness to diagnosis
Multiple comorbidities are associated with pediatric psoriasis