Genetic testing at Cleveland Clinic provided patient with an updated diagnosis
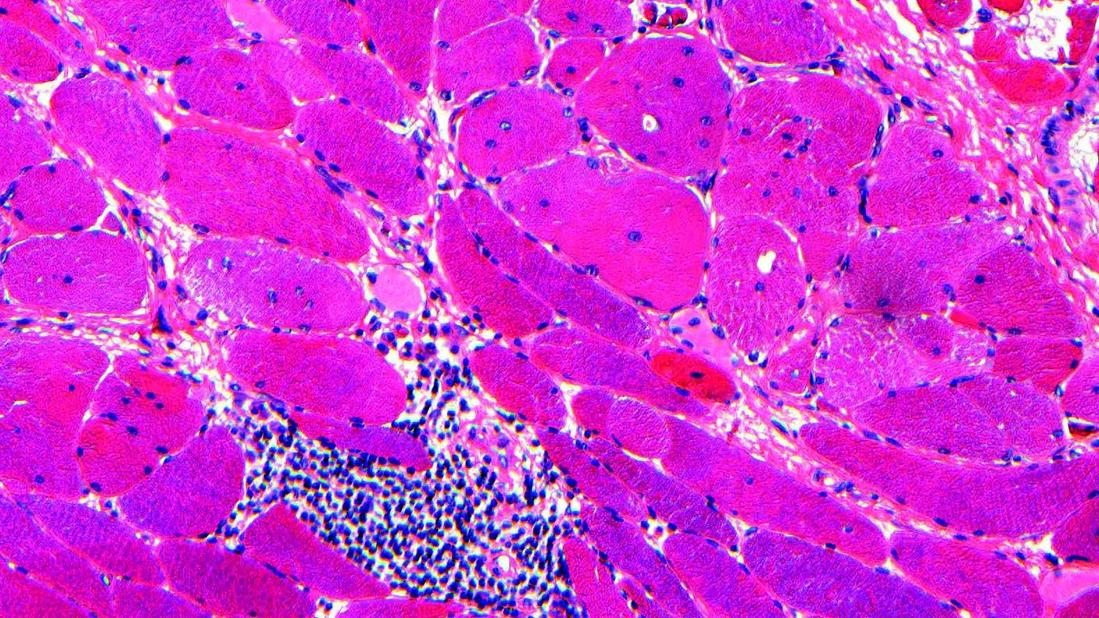
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b10fcf9c-7e90-456b-b132-5511bf1bf547/muscle-biopsy-cells-indicating-myositis)
Muscle biopsy slide image showing myositis
By Jennifer Elise Abdalla, MD, and Ambreesh Chawla, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 45-year-old female who was diagnosed with juvenile myositis in the 1980s presented to our rheumatology clinic for further evaluation of inflammatory myositis. Her symptoms began at age 7, when she had hand weakness and difficulty rising from a chair in conjunction with recurrent falls, and she ultimately required use of a wheelchair. She also exhibited a toe-walking gait, which led to Achilles tendon-lengthening surgery. A muscle biopsy of her calf performed at the time noted “polymyositis,” and for many years she was treated for presumed juvenile polymyositis with prednisone, methotrexate and mycophenolate mofetil. Her creatine kinase (CK) level ranged from 200 U/L to a maximum of 583 U/L (reference range 42-196 U/L). Upon examination, she displayed diffuse, symmetric weakness of both proximal and distal muscle groups as well as bilateral elbow contractures.
Given the atypical features of her case — specifically distal muscle involvement, mildly elevated CK levels < 1000 U/L, and joint contractures — the diagnosis of inflammatory myositis was reconsidered. She was referred to Cleveland Clinic’s Neuromuscular Medicine Clinic, where genetic testing corroborated the diagnosis of Bethlem myopathy.
This rare congenital muscular dystrophy is caused by a mutation in the COL6A gene, which encodes a critical component of type VI collagen. Bethlem myopathy is characterized by early-onset muscle weakness, typically in the first or second decade of life, along with increased distal joint laxity, joint contractures and muscle-tendon contractures.
Advertisement
The disease progresses slowly, and CK levels are often normal or mildly elevated. Many patients eventually require assistive devices.1 Inherited muscular
dystrophies such as Bethlem myopathy sometimes can be misdiagnosed as idiopathic inflammatory myopathies (IIM), as both conditions can present with proximal muscle weakness.
IIM, also known as myositis, is a heterogeneous group of autoimmune disorders that can be classified into multiple subgroups: dermatomyositis, polymyositis,
anti-synthetase syndrome, immune-mediated necrotizing myopathy and overlap myositis. These conditions are relatively rare, with an incidence of 0.2-2 per 100,000 person-years and an annual prevalence of 2-25 per 100,000 individuals.2
IIM typically presents over weeks to months with symmetric weakness affecting the proximal muscles of both the upper and lower extremities. Laboratory tests usually show a significant elevation in CK levels (often > 1,000 U/L) and the presence of myositis-specific antibodies in 50% to 60% of cases.3
Several conditions can present with muscle weakness that may mimic IIM, including (but not limited to) muscular dystrophies, metabolic myopathies,
mitochondrial myopathies, and toxic or endocrine-related myopathies.
This case highlights the importance of differentiating between these conditions and IIM to avoid unnecessarily exposing patients without IIM to systemic immunosuppressive treatments. Obtaining and performing a comprehensive medical history, physical examination, laboratory/serologic workup, electromyography, muscle biopsy and genetic testing are often critical to avoid an incorrect diagnosis.
Advertisement
Certain clinical features that are incongruent with IIM and might point to an alternative diagnosis include slow evolution of weakness over years, family history of muscle weakness, asymmetrical weakness and predominantly distal muscle weakness.
1. Silverstein RS, Wang DD, Haruno LS, Lotze TE, Scott AC, Rosenfeld SB. Bethlem Myopathy (Collagen VI-Related Dystrophies): A Retrospective Cohort Study on Musculoskeletal Pathologies and Clinical Course. J Pediatr Orthop. 2023 Feb 1;43(2):e163-e167.
2. Khoo T, Lilleker JB, Thong BY, Leclair V, Lamb JA, Chinoy H. Epidemiology of the idiopathic inflammatory myopathies. Nat Rev Rheumatol. 2023 Nov;19(11):695-712.
3. Ghirardello A, Zampieri S, Tarricone E, et al. Clinical implications of autoantibody screening in patients with autoimmune myositis. Autoimmunity. 2006;39(3):217-221.
Advertisement
Advertisement
As genetic insights refine diagnosis, research abounds on current and emerging therapies
Advances in imaging technology could offer new insights for combatting age-related muscle loss
Unraveling the TNFA receptor 2/dendritic cell axis
Nasal bridge inflammation, ear swelling and neck stiffness narrow the differential diagnosis
Findings show profound muscle loss variance between men and women
From dryness to diagnosis
Multiple comorbidities are associated with pediatric psoriasis
Untreated seropositive erosive RA led to peripheral ulcerative keratitis