Taking a combined surgical/electrophysiology strategy to the next level
Convergent, the hybrid epicardial/endocardial approach to atrial fibrillation (AF) ablation, is increasingly used to provide a more durable and reliable posterior wall isolation with significantly reduced risk of esophageal injury. “Convergent Plus” adds ablation of the ligament of Marshall and a left atrial appendage (LAA) clip to further reduce stroke risk and AF burden. This more complete strategy has been pioneered at Cleveland Clinic and is now offered at its Complex AF Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Surgeons and electrophysiologists each bring unique capabilities to the table to optimize strategies for persistent AF,” says Ayman Hussein, MD, Medical Co-Director of Cleveland Clinic’s Atrial Fibrillation Center. “The collaborative hybrid approaches are improving outcomes while reducing risks.”
While excellent outcomes can typically be achieved with endocardial catheter ablation alone in patients with paroxysmal AF, success rates for a first-time procedure for persistent AF tend to be only around 65%.
Dr. Hussein explains that AF is mainly paroxysmal early in its course, with triggers from the pulmonary veins being the main culprit. As time goes on, the role of the substrate becomes increasingly important as the left atrium changes: mechanical stress due to pericardial tethers and cardiac motion causes stress-induced inflammation, leading to fibrosis and increased susceptibility to fibrillation, especially along the posterior wall.
“Many strategies have been tried to improve the outcomes of ablation in patients with persistent AF with only modest success,” says Walid Saliba, MD, Director of Cleveland Clinic’s Electrophysiology Lab and Medical Co-Director of the Atrial Fibrillation Center. He identifies several likely explanations:
Advertisement
The multicenter CONVERGE (Convergence of Epicardial and Endocardial Ablation for the Treatment of Symptomatic Persistent AF) trial compared efficacy and safety of adding epicardial left atrial posterior wall ablation (conducted by a cardiac surgeon) to endocardial catheter ablation to isolate the pulmonary veins (conducted by an electrophysiologist). Results were published in late 2020 in Circulation: Arrhythmia and Electrophysiology.
Freedom from atrial arrhythmia absent new or increased medications was reached at 12 months in 67.7% of patients who underwent the hybrid approach versus 50.0% of those who received endocardial catheter ablation alone (risk ratio = 1.35; P = 0.036). Off-antiarrhythmic drug success was achieved in 53.5% versus 32.0%, respectively (risk ratio = 1.67; P = 0.013). No deaths, cardiac perforations or atrioesophageal fistulas occurred.
“The hybrid Convergent procedure needs no cardiopulmonary bypass, and it spares the sternum and protects the esophagus,” says Cleveland Clinic cardiothoracic surgeon Edward Soltesz, MD, MPH, Surgical Co-Director of the Atrial Fibrillation Center. “By targeting triggers and substrate, it provides a viable treatment option for complex atrial fibrillation.”
Cleveland Clinic’s Complex AF Clinic offers state-of-the-art mapping and ablation techniques for patients with challenging AF cases, especially those who failed prior ablation procedures.
The epicardial ablation of the posterior wall is conducted first by a cardiothoracic surgeon via subxiphoid or transdiaphragmatic access to the pericardium. The posterior left atrium contributes minimally to left atrial ejection, Dr. Soltesz explains, with multiple studies demonstrating little ill effect of complete ablation.
Advertisement
Next, the endocardial procedure is conducted by an electrophysiologist in standard fashion.
The “plus” indicates additional management with a thoracoscopic LAA clip and ligament of Marshall ablation.
“Applying a left atrial appendage clip may have benefits in terms of both stroke prevention and arrhythmia control,” says Oussama Wazni, MD, Section Head of Cardiac Electrophysiology and Pacing at Cleveland Clinic.
He notes that LAA clipping is one of the main advantages of Convergent Plus, citing the recently published Left Atrial Appendage Occlusion Study (N Engl J Med. 2021;384:2081-2091). In patients who underwent surgery for AF, closing the appendage led to reduced incidence of stroke or systemic embolism after a mean follow-up of 3.8 years relative to those who did not have LAA closure (4.8% vs. 7.0%, respectively; hazard ratio = 0.67; 95% CI, 0.53-0.85; P = 0.001).
“We also target the ligament of Marshall because that has been shown to contribute to atrial fibrillation physiology in many cases,” Dr. Wazni adds.
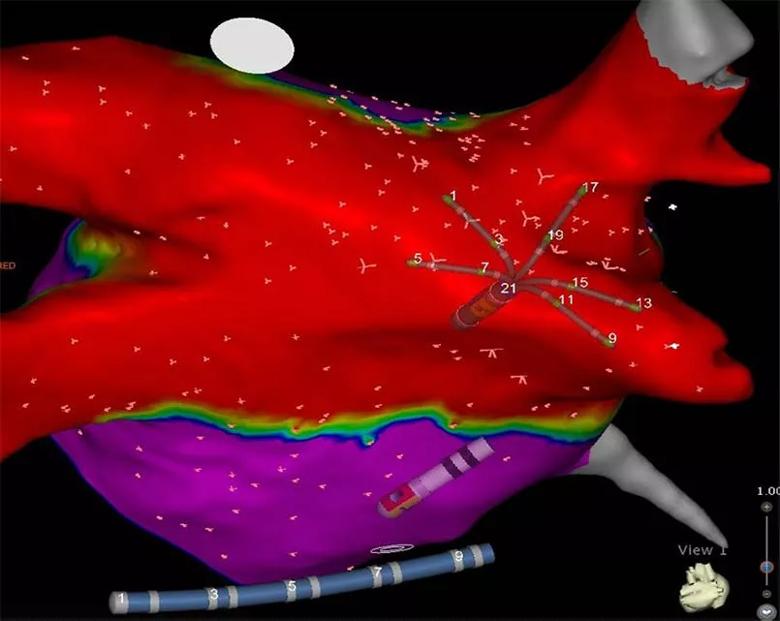
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1d719130-5fb5-4bfa-bcf8-0d446f63010d/21-HVI-2282758-Inset-New-805x641-12_jpg)
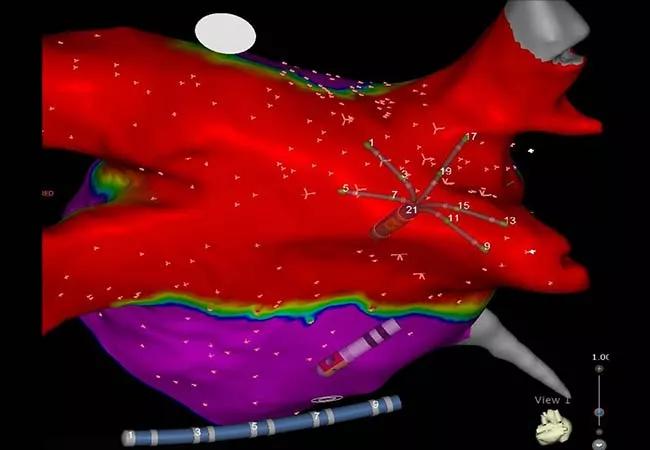
A map of the left atrium showing electrical isolation (red) of the pulmonary veins and the posterior wall that is characteristic of results with the Convergent Plus procedure.
Patients with any of the following should be considered for a hybrid procedure:
Absolute contraindications are either a documented LAA thrombus or significant valvular or coronary heart disease. These findings should prompt an open surgical approach and a concomitant Cox-Maze IV lesion set.
Advertisement
Hybrid procedures can be performed staged or in a single day. “At Cleveland Clinic, we prefer a staged approach, which allows resolution of postsurgical acute edema before the endocardial procedure is started,” Dr. Soltesz notes. “It also enables the epicardial lesions to mature.”
Moreover, he adds, staging allows time to determine whether a patient actually needs a second procedure, which can be helpful for patients who have had prior catheter ablations with good control of the pulmonary veins.
Cleveland Clinic’s Complex AF Clinic also has a research component: prospective data on patient characteristics and outcomes are collected, with the goal of assessing new technologies.
Dr. Saliba identifies several issues that deserve further research:
“Our Complex AF Clinic presents a great opportunity to move science forward,” Dr. Hussein concludes. “We anticipate that we’ll soon have longitudinal data on patient outcomes to share.”
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more