Addressing an extreme case
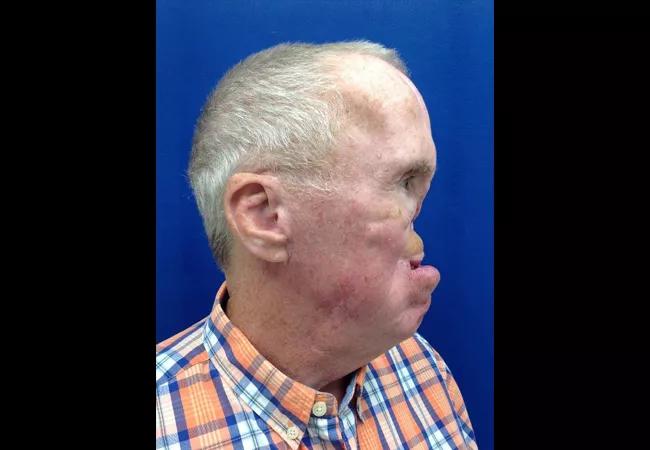
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/97c3372a-31f9-4edc-9e36-eed1c459f1e1/18-ENT-545-Karunagaran-Hero-Image-650x450pxl_jpg)
18-ENT-545-Karunagaran-Hero-Image-650x450pxl
Rehabilitation of patients with head and neck defects or disabilities caused by development, trauma or disease requires specialized care among several disciplines.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Adults and children with melanoma or carcinoma, birth defect patients with craniofacial deformities (specifically microtia), and car accident patients suffering orofacial injuries often need the comprehensive skills of a team of specialists in Cleveland Clinic’s Head & Neck Institute, including neck surgeons, oral surgeons, general and specialty dentists. They often work with plastic surgeons, radiation oncologists, speech language pathologists and anaplastologists to restore form and function – and a sense of normalcy – to patients with intraoral and extraoral defects.
The teaming of Sanjay Karunagaran, DDS, MSD, a prosthodontist, and Theodore R. Arlotto, MAMS, an anaplastologist, in the Maxillofacial Prosthodontic Clinic in the Head & Neck Institute provides a unique skill set in creating custom prostheses to replace missing areas of bone or tissue that can restore oral function, such as swallowing, speech and chewing.
“Patients with intraoral or facial issues are interested in getting back to a more normal existence – being able to eat, talk normally, go out in public and interact with people,” Arlotto says. “It can be a self-confidence booster. Someone who doesn’t want to go back to work because they lost an ear or an eye can get a prosthesis that can help them get back out in the world and living a more normal life.”
Dr. Karunagaran says he sees patients on the extreme end of the spectrum who require specialized care.
Extraoral prostheses can include ocular, orbital, auricular, nasal and midfacial prostheses. Intraoral prostheses can include:
Advertisement
“Many patients can’t be reconstructed surgically,” Dr. Karunagaran says. “While surgery can do a lot of things, in order for some patients to be fully functional they need a prosthetic.”
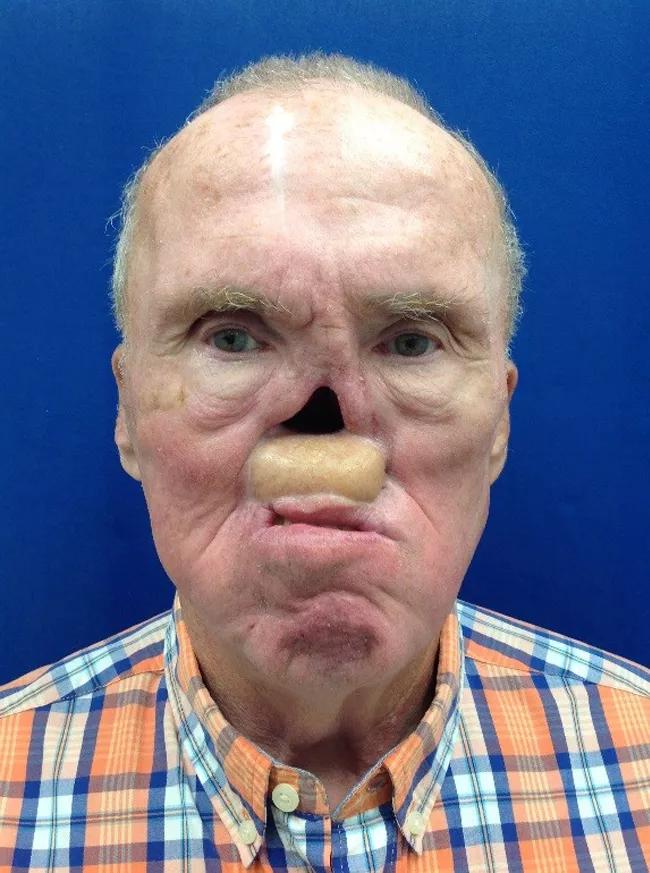
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c90df2d8-9090-46f8-9064-e9422cd41916/18-ENT-545-Karunagaran-Inset-Image-650pxl-width_jpg)
In one recent case, a patient came in for a prosthodontic dental procedure when the team noticed he was missing a nose from previous treatment for squamous cell carcinoma of the nasal cavity. The nose was resected and followed up with radiation therapy.
The patient avoided wearing his original prosthesis because it was too large, the coloring was off and he had difficulty keeping his glasses on his face. As a result, he rarely wore the device, opting for a bandage over the defect and avoiding public appearances.
Dr. Karunagaran and Arlotto worked with the patient to create a prosthesis that extended back into the defect site and locked into the undercut areas for retention.
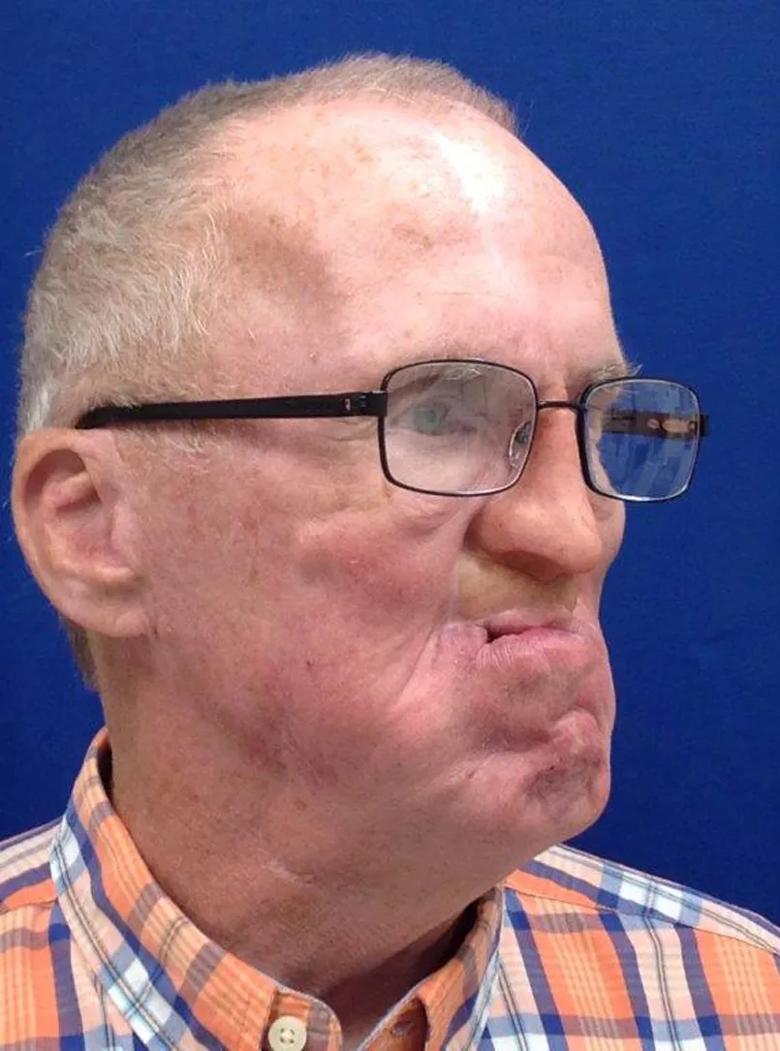
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a26bd524-45ac-49c9-a463-018184151939/18-ENT-545-Karunagaran-Inset-Image-02-805pxl-width_jpg)
“We were able to work with the natural shape of the tissue and design a prosthesis that can be locked in place without adhesive,” Arlotto says. The prosthesis was custom stained and colored to fit the patient’s existing skin tone, resulting in a happy patient who wears the prosthesis in public and reports improvement in his physical and mental well-being.
The process works by taking impressions of the defect site, molding a wax prototype, making adjustments based on patient feedback, and creating the final silicone prosthetic. The timeline for completion varies form case to case, but extraoral prostheses can take months to create and refine, while intraoral prostheses can take up to two years for completion. Ocular prostheses, for example, can be completed in three to four weeks, while a facial prosthesis can take four to seven weeks.
Advertisement
Follow-up depends on the patient’s needs. A patient receiving a prosthesis for the first time, or who has little support at home, may require multiple appointments and fittings, while someone who has had a prosthesis in the past will need less follow-up care.
While Dr. Karunagaran and Arlotto tend to see patients after surgery, they say meeting with a patient after diagnosis, but prior to surgery, provides the ability to pull an impression from an ear or nose and create a prosthesis that closely matches the natural face. When that isn’t possible, Arlotto works from photographs or tries to match the non-affected orbit or ear.
“There are many people who need these extra oral devices to help them gain their confidence and happiness so they are able to function normally in society,” says Dr. Karunagaran. “Many times, patients are not aware that our team is here and doing this type of work. Our goal is to make more physicians and patients aware of the service we provide.”
Advertisement
Advertisement
Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor
Case study illustrates the potential of a dual-subspecialist approach
Evidence-based recommendations for balancing cancer control with quality of life
Study shows no negative impact for individuals with better contralateral ear performance
HNS device offers new solution for those struggling with CPAP
Patient with cerebral palsy undergoes life-saving tumor resection
Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition
Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.