Vigilant MRI evaluation needed for prompt care of potentially reversible inflammation, study finds
In patients with cerebral amyloid angiopathy (CAA), radiological evidence of related inflammation is relatively common and most cases may go undetected and untreated, concludes a database study from Cleveland Clinic researchers published in the Journal of Stroke and Cerebrovascular Diseases (2023 Oct 26;32[12]:107436).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Ours is the first study spotlighting the high prevalence of underrecognized or undiagnosed radiological and possibly clinico-radiological CAA-related inflammation in patients with radiological CAA,” says corresponding author G. Abbas Kharal, MD, MPH, a vascular neurologist in Cleveland Clinic’s Cerebrovascular Center. “Vigilant radiological evaluation to detect CAA-related inflammation in patients with underlying CAA may enable earlier detection of the reversible and treatable inflammation associated with CAA and ultimately reduce cognitive decline and seizure risk in these patients.”
CAA is a small-vessel vasculopathy most often diagnosed after age 50. It is caused by deposition of abnormal amyloid proteins in the walls of small vessels in the brain and leptomeninges. The resulting vessel wall thickening, hyalinization and damage typically lead to clinical and neuroradiological findings that include intracerebral hemorrhage, cognitive impairment and transient focal neurologic deficits.
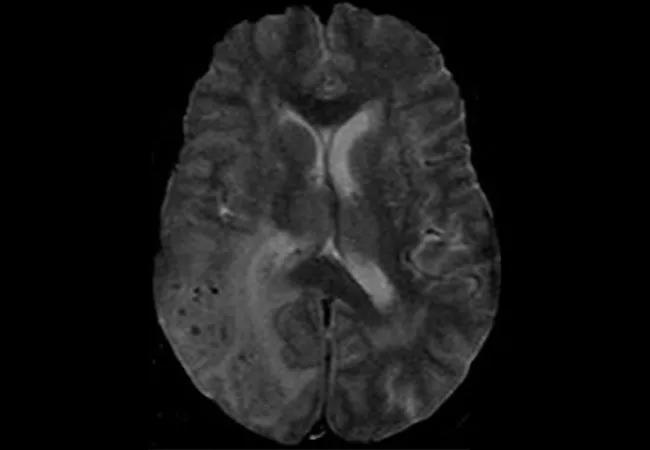
Some patients with CAA develop a T-cell-mediated inflammatory reaction to the vascular amyloid deposition, resulting in CAA-related inflammation (CAA-RI). On MRI, the perivascular inflammation characteristic of CAA-RI is seen as vasogenic edema in regions of perivascular amyloid deposition and leptomeningeal enhancement. The exact mechanism of CAA-RI is unknown, but evidence suggests that it has an autoimmune basis related to antibodies targeted against the amyloid-beta protein.
Few studies have been published about CAA-RI, and none of the existing reports have accounted for subclinical CAA-RI, which may manifest on brain imaging but produce no significant symptoms. Therefore, the true prevalence of the condition is unknown.
Advertisement
To help fill that knowledge gap, Dr. Kharal and colleagues performed a retrospective review of electronic medical records to determine the prevalence of radiological CAA-RI among patients with CAA and to characterize these patients’ presenting clinical features.
The researchers identified 1,100 patients aged 50 or older with a diagnosis of amyloidosis or CAA who presented to multiple centers within Cleveland Clinic from January 2010 through June 2020. Of these, 511 patients had appropriate brain MRI findings available that met radiological modified Boston 2.0 criteria for possible or probable CAA; this cohort made up the study’s overall CAA population.
Among these 511 patients, 193 also had white matter hyperintensity (WMH) on MRI disproportionate to microvascular ischemic disease. Brain MRIs from these 193 patients were analyzed by a vascular neurologist and then by a neuroradiologist — both of whom were blinded to clinical information — to assess for compatibility with imaging criteria for radiological possible or probable CAA-RI (based on the presence of WMH lesions extending to the immediate subcortical white matter and WMH asymmetry).
Clinical features such as macrohemorrhages and interval silent ischemic infarcts were also reviewed, as were patient outcomes. Symptoms of CAA-RI include subacute cognitive decline, headaches and seizures. “Current diagnostic criteria for the condition include presence of CAA on brain MRI, clinical features suggestive of CAA-RI, age greater than 40 years, asymmetric white matter hyperintensity and exclusion of mimics,” notes Dr. Kharal.
Advertisement
Review by the vascular neurologist and neuroradiologist identified 55 patients deemed to have brain MRI findings compatible with radiological possible (n = 21) or probable (n = 34) CAA-RI, representing 10.8% of the overall CAA population and 28.5% of patients with CAA and WMH. The prevalence of radiological probable CAA-RI alone was 6.6% in those with CAA and 17.6% in those with CAA and WMH.
Only 10 (18.2%) of the 55 patients with MRIs suggestive of radiological possible or probable CAA-RI were initially diagnosed with the condition, and 20 (36.4%) were diagnosed during monitoring that continued up to 74 months later.
A majority of patients with radiological CAA-RI were women (61.8%). Mean age at the time that radiological CAA-RI findings developed was 72.9 years. Cerebrospinal fluid studies at the time of CAA-RI development on MRI revealed no or very little inflammation. However, 96.4% of patients with radiological CAA-RI had at least one clinical symptom of CAA or CAA-RI.
“Many of these symptoms were present at baseline, before development of radiological possible or probable CAA-RI, but the percentages were higher when patients were diagnosed with CAA-RI,” Dr. Kharal notes. “This suggests there could be a prodromal period before the emergence of neuroradiological CAA-RI findings.”
The most common concomitant symptoms at the time of the earliest MRI findings of probable CAA-RI were cognitive impairment (74.5%), macrohemorrhages (52.7%), headache (30.9%), seizures (14.5%) and ischemic infarcts (14.5%).
Advertisement
Eighteen (32.7%) of the 55 patients with radiological possible or probable CAA-RI had been treated with immunosuppression. While no treatment to date has been shown to reduce recurrent hemorrhage risk in patients with CAA or related inflammation, patients treated with immunosuppression in this study had a noticeable decline in the incidence of new macrohemorrhages. The researchers note that this may be related to arterial wall changes related to the immunosuppression but that further studies with larger samples are needed to validate this and their other findings.
The investigators conclude with an observation about the timeliness of their study: “Given the overlap of CAA and Alzheimer’s disease,” they write, “these findings may also be relevant in patients with amyloid-related imaging abnormalities.”
Image at top: Brain MRI of a patient at the time of CAA-RI diagnosis. Reprinted from Amin et al., “The prevalence of radiological cerebral amyloid angiopathy-related inflammation in patients with cerebral amyloid angiopathy,” Journal of Stroke and Cerebrovascular Diseases (2023 Oct 26;32[12]:107436), © 2023, with permission from Elsevier.
Advertisement
Advertisement

Exploring new tools and techniques to improve the diagnosis and treatment of concussions.

Training, tools and resources lead to safer, more compassionate care

Cleveland Clinic researchers collaborate with Microsoft to create a product ready for the field
New research sheds light on a potentially devastating condition that is reversible when properly managed

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

Unraveling the TNFA receptor 2/dendritic cell axis

Nasal bridge inflammation, ear swelling and neck stiffness narrow the differential diagnosis

Genetic testing at Cleveland Clinic provided patient with an updated diagnosis