In experienced hands, up to 95% of patients can be free of reoperation at 15 years
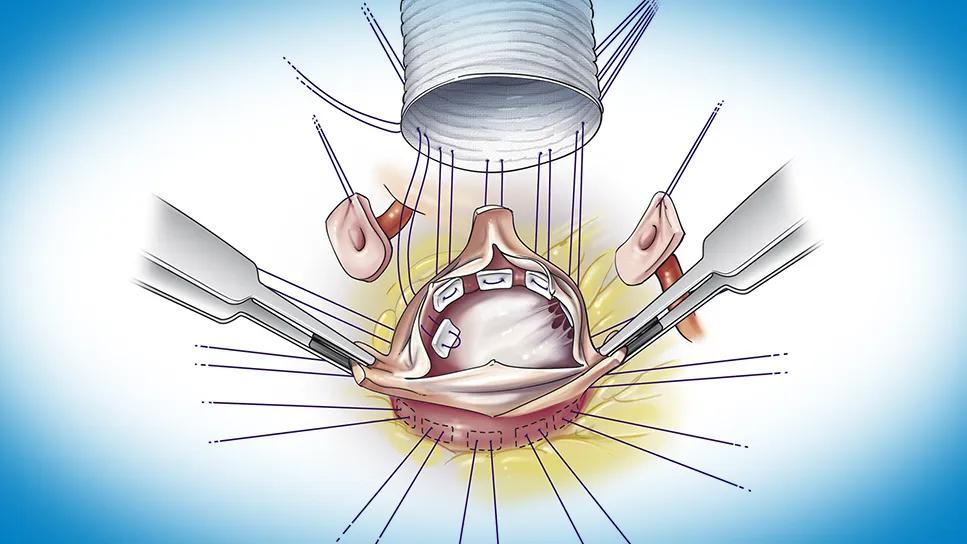
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4adaec06-dd9b-449e-9595-968d75c78899/valve-sparing-root-replacement-feature)
illustration of a stent graft being surgically placed on a heart valve
Patients who require aorta surgery for a dilated aorta or aortic root often have some degree of aortic valve regurgitation as well. At Cleveland Clinic, these patients frequently are offered aortic valve repair in combination with aortic root replacement with valve reimplantation, also known as valve-sparing aortic root replacement.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Not all cardiovascular providers recognize how often the aortic valve can be repaired with really good results at a highly experienced center,” says cardiothoracic surgeon Lars Svensson, MD, PhD, Chief, Cleveland Clinic Heart, Vascular and Thoracic Institute. “And the best results are achieved when repair is done with a reimplantation operation, which can achieve rates of freedom from reoperation over 10 to 15 years comparable to those with mitral valve repair. We currently perform concurrent aortic valve repairs in about 20% to 25% of our reimplantation operations.”
“We most often perform valve-sparing root replacement in patients who have no more than mild or moderate aortic regurgitation with an aneurysmal root,” notes Milind Desai, MD, MBA, Medical Director of Cleveland Clinic’s Aorta Center and a cardiologist in its Valve Center. “A small amount of calcium can be surgically removed from the valve if present, but the valve typically needs to be free of advanced stenosis or significant regurgitation to qualify for repair. These are generally younger patients in whom we want greater durability than a bioprosthesis can deliver without the lifelong anticoagulation required with a mechanical valve.”
The reimplantation operation (Figure) involves mobilizing the aortic valve, putting pledgets in the left ventricular outflow tract (LVOT), placing the valve inside a tube graft to replace the aortic root, sewing the graft into position and hooking it to the coronary arteries. Dr. Svensson performs the operation using modifications he made to the David reimplantation method more than 20 years ago, with the goal of improved durability. Essential features of his modified technique include:
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/481595e3-4ca7-4dd2-82ff-6bed8078bcb3/valve-sparing-root-replacement-inset)
Figure. Key steps in the modified valve-sparing aortic root replacement procedure. (A) The aortic valve is mobilized so the entire annulus can be housed within the tube graft. Valve sutures are passed from inside the ventricular outflow tract and through the polyester tube graft. (B) The sutures are tied down around a Hegar dilator appropriate to the patient’s body surface area, and the valve is sewn into position within the graft. (C) The coronary artery ostia buttons, buttressed by felt, are attached to the side of the graft. Reprinted from the Journal of Thoracic and Cardiovascular Surgery (2022;163:51-63), Mokashi et al., ©2020, with permission from the American Association for Thoracic Surgery.
The reimplantation operation makes repair — and thus preservation of the native valve — possible in more patients, especially those with more severe regurgitation, Dr. Svensson says. “Using the reimplantation operation in patients with severe aortic regurgitation without a particularly large root gives me much more control in repairing the valve leaflets, providing a leg up in preserving three-leaflet valves,” he explains.
In fact, he adds, in recent years Cleveland Clinic has increasingly used the reimplantation operation for leaking valves in patients with small aortic roots, i.e., < 4.5 cm. Enough experience has been accumulated in this small-root population that Dr. Svensson and colleagues have completed a study (not yet published) showing good results in these patients in terms of operative success, survival and freedom from reoperation. “Very few people are doing these procedures in patients with such small roots, so we hope to provide some insight and guidance,” he notes.
Dr. Svensson adds that bicuspid aortic valves require slightly different techniques than those used for trileaflet valves, but the same principles apply to both valve types in this setting.
“I tell patients with trileaflet valves that there’s a 95% chance we can preserve their native valve, particularly if their root is enlarged,” he says. “For patients with a bicuspid valve, the chance is about 80%. Although that’s still good, it’s lower because bicuspid valves are more likely to have severe calcification that cannot be seen on echocardiography but is apparent during surgery, which means the valve needs replacing.”
Advertisement
The importance of detecting significant valve calcification or holes in valve leaflets makes highly precise imaging imperative in these patients, whether they have trileaflet or bicuspid valves.
“In most of these patients we obtain a gated contrast CT scan to get precise measurements of the root of the annulus and where the coronary arteries lie,” Dr. Desai says. “We also obtain echocardiograms and, in some cases, transesophageal echocardiograms to ensure there is no significant calcification of the valve and that the leakage is not so significant to rule out repair.
“The timing of most valve-sparing root replacements is driven by concern about aortic root aneurysm,” Dr. Desai continues. “So the imaging-based valve assessment needs to be precise enough to determine whether the valve’s condition, in terms of leakage severity and stenosis, allows for repair rather than replacement within that timetable driven by the root disease.”
Over the past quarter century, Cleveland Clinic has accumulated the world’s largest experience in valve-sparing aortic root replacements, enabling publication of some of the most extensive observational research on these procedures in the literature, which demonstrates excellent outcomes for patients.
For instance, a recent report of long-term outcomes in 491 adults undergoing elective modified aortic valve reimplantation found 95% freedom from aortic valve reintervention at 15 years (J Thorac Cardiovasc Surg. Epub 2024 Aug 22). There were no operative deaths, and survival at 15 years was 87%.
Advertisement
Another recent study in 756 patients with trileaflet valves undergoing modified reimplantation showed that the need for cusp repair at the time of reimplantation does not affect long-term hemodynamic or clinical outcomes (JTCVS Open. 2023;161:105-122). Across the cohort, 10-year freedom from reoperation was the same — 97% — regardless of whether patients underwent reimplantation with cusp repair or without it. “The need for cusp repair should not deter surgeons from performing a valve-sparing operation,” Dr. Svensson and his Cleveland Clinic co-authors concluded.
In the two studies above, most patients had trileaflet aortic valves. The Cleveland Clinic experience has shown outcomes of valve-sparing root replacement with bicuspid valves to be comparable to those with trileaflet valves through five years; over longer follow-up, however, bicuspid valves have been associated with a somewhat higher rate of valve reoperations, requiring closer surveillance over time (J Thorac Cardiovasc Surg. 2022;163[1]:51-63). “At an experienced center, valve-sparing root replacement for aortic aneurysm can be an attractive option for appropriate patients with either a trileaflet or a bicuspid valve,” Dr. Svensson says, “but bicuspid anatomy calls for extra vigilance in patient selection and long-term follow-up.”
Indeed, careful lifelong surveillance is essential in all cases of valve-sparing aortic root replacement, given the need for lifetime management of aortic disease. Its importance in this specific setting was highlighted by a Cleveland Clinic study of 756 patients with trileaflet valves who underwent valve-sparing root replacement (J Thorac Cardiovasc Surg. 2024;167[1]:101-111). It found that although long-term survival was similar between patients who did and did not have residual aortic regurgitation at discharge, the risk of reoperation was significantly higher if residual regurgitation was present. “This underscores that complete elimination of regurgitation by a skilled surgeon is essential for long-term success,” notes Dr. Svensson.
Advertisement
“This study also shows that it’s critical to follow patients found to have residual regurgitation extra closely to ensure prompt recognition of any need for reoperation,” adds Dr. Desai. “Moreover, this study’s finding that the risk of residual regurgitation at discharge was associated with severity of preoperative regurgitation argues for early referral to an experienced center for valve-sparing root replacement. That appears to give patients the best chance of long-term regurgitation-free survival.”
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
Surgeons credit good outcomes to experience with complex cases and team approach
For many patients, repair is feasible, durable and preferred over replacement
Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach
20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation