Many young patients can avoid lifelong anticoagulation with a valve-sparing approach
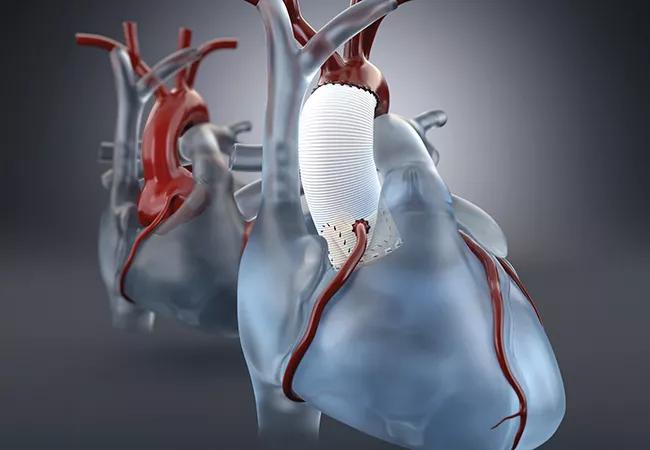
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6861e2d2-f55c-45f7-be18-1b91095cc6b5/23-HVI-4417336-CQD-650x450-1_jpg)
23-HVI-4417336 CQD 650×450
Patients with Marfan syndrome or other connective tissue disorders (CTDs) often require prophylactic aortic root replacement at a relatively young age, yet there has been uncertainty about how durable reimplanted myxomatous aortic valves are in these individuals. Now a new study from Cleveland Clinic offers reassurance about the long-term durability of valve-sparing approaches in this complex patient population.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Treatment decisions in these patients — whether to replace the aortic valve or attempt repair and a valve-sparing approach — carry lifelong ramifications,” says the study’s lead author, Lars Svensson, MD, PhD, Chief, Cleveland Clinic Heart, Vascular & Thoracic Institute, and Surgical Director of the Cardiovascular Marfan and Connective Tissue Disorder Clinic. “Our data show that valve reimplantation in this setting is associated with excellent event-free survival and valve function through at least 10 years while freeing patients of the established risks of anticoagulation that come with mechanical composite valve grafts.”
The current study (J Thorac Cardiovasc Surg. 2023;166:1617-1626) extends and expands upon an earlier series in 178 Cleveland Clinic patients with CTDs published by Dr. Svensson and colleagues in 2013. That analysis showed that prophylactic root and valve preservation using David reimplantation was safe and provided excellent midterm effectiveness with a low risk of late events.
In the updated series, the investigators retrospectively analyzed patients who underwent elective aortic valve reimplantation surgery at Cleveland Clinic up to 2020. Of these, 214 had a CTD and 645 did not. The CTD cohort consisted of 164 patients (77%) with Marfan syndrome, 23 (11%) with Loeys-Dietz syndrome, seven (3%) with Ehlers-Danlos syndrome and 20 (9%) with other CTDs.
Patients with CTDs were significantly younger than those without CTDs (mean age of 39 vs. 53 years) and were more likely to be women, less likely to have aortic regurgitation, and more likely to have mitral valve regurgitation, left ventricular dysfunction and chronic obstructive pulmonary disease.
Advertisement
To adjust for differences between the two groups, 96 CTD patients were matched to 96 non-CTD patients using propensity scores. Outcomes were compared over follow-up that continued beyond 15 years in some patients and for more than nine years in 25% of the cohort.
Results in the overall CTD cohort. Among the overall cohort of 214 patients with a CTD, initial results were excellent, with no operative deaths, one stroke (0.47%) and one early valve reoperation (0.47%). Over longer follow-up, 97% of patients remained free from valve reoperation at five years and 95% at 12 years. All reoperations (n = 5) were among patients with Marfan syndrome. Survival was 96% at five years and 92% at 12 years. At 10-year echocardiographic follow-up, 86% of patients had no aortic regurgitation, 11% had mild regurgitation and 3% had moderate regurgitation.
“These findings all compare favorably to those in the general reimplantation population,” Dr. Svensson notes.
Comparative results from the propensity-matched cohorts. In the propensity-matched cohorts, there were no significant differences between the groups with and without CTDs in terms of in-hospital outcomes, longitudinal aortic regurgitation and mean gradient, risk of aortic valve reoperation or risk of late death. Notably, 10-year freedom from aortic valve reoperation was numerically higher in the CTD group than in the non-CTD group (98% vs. 93%; P = 0.3).
“These long-term results help validate aortic valve reimplantation as a durable option with low rates of valve deterioration in patients with connective tissue disorders,” says Dr. Svensson. “Freedom from reoperation compared favorably even to published outcomes with mechanical valve grafts.”
Advertisement
The authors attribute the excellent durability to proper patient selection aimed at avoiding use of valves with large fenestrations. They note that intraoperative assessment of leaflet pathology and fenestrations is critical in selecting appropriate candidates. Downsizing annular dimensions to normal by use of a Hegar dilator also likely optimized cusp coaptation.
“After weighing the need for lifelong anticoagulation and risk of bleeding with mechanical valves, many patients with connective tissue disorders should consider an attempt at valve repair when undergoing root replacement if acceptable valve tissue is present,” Dr. Svensson observes.
The authors note that a randomized trial comparing reimplantation with composite valve grafts would be ideal for determining the best approach for patients with CTD, although the likelihood of such a study is highly uncertain. And they caution that the results they report may differ at lower-volume centers without Cleveland Clinic’s extensive experience with aortic valve reimplantation, given the complexity of the operation, particularly in the setting of tissue fragility often seen with CTDs.
“Regardless of the surgical approach taken, close lifelong echocardiographic monitoring is required in this high-risk patient population,” adds co-author Vidyasagar Kalahasti, MD, a cardiologist who serves as Medical Director of Cleveland Clinic’s Cardiovascular Marfan and Connective Tissue Disorder Clinic. “Even so, valve-sparing aortic root replacement is a game changer for patients with connective tissue disorders, as it allows aortic valve preservation without the patient needing to take anticoagulation or suffer early bioprosthetic valve degeneration.”
Advertisement
“These real-world data provide reassurance that we can achieve lasting outcomes when reimplanting valves in suitable patients with connective tissue disorders,” Dr. Svensson concludes. “While lifelong imaging follow-up is still needed, we can tell appropriate patients that bioprosthetic and mechanical valve options may not offer advantages over preserving their native aortic valve.”
Advertisement
Advertisement
When to recommend aortic root surgery in Marfan and other syndromes
Cleveland Clinic’s Rheumatic Lung Disease program treats patients with complex conditions
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Series of 145 patients characterizes scope of presentations, interventions and outcomes
Experience-based takes on valve-sparing root replacement from two expert surgeons
New review distills insights and best practices from a high-volume center
Recent Cleveland Clinic experience reveals hundreds of cases with anatomic constraints to FEVAR
Least-invasive open-heart AVR option to date yielded rapid recovery in all cases