A testament to multidisciplinary collaboration
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A previously healthy 20-year-old woman was transferred to Cleveland Clinic’s medical intensive care unit for management of severe acute respiratory distress syndrome (ARDS) secondary to post-influenza cavitatory S. aureus pneumonia. Her hospital course prior to the transfer was complicated by acute respiratory failure requiring mechanical ventilation and tracheostomy, right-sided pneumothorax necessitating pigtail catheter insertion, septic shock requiring vasopressor support, sepsis-induced cardiomyopathy and acute kidney injury. Transfer occurred on Day 20 of admission.
Computed tomography (CT) of the chest revealed dense consolidation and large cavities bilaterally.
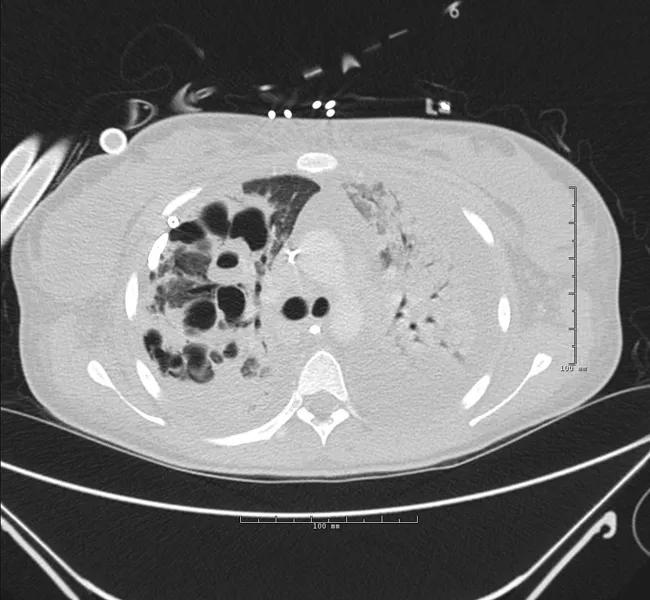
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c81ef06a-5ec1-43c8-8036-95ca832cdfa7/18-PUL-4873-Krishnan-Inset-Image-01-650pxl-width_jpg)
CT scan on day 1 of hospital transfer.
Her condition deteriorated precipitously within 24 hours of arrival despite optimal conventional medical management. She was emergently cannulated at the bedside for venovenous extracorporeal membrane oxygenation (VV-ECMO) for refractory hypoxemia and unsafe inflation pressures on mechanical ventilation. We chose a dual-site (internal jugular return cannula, femoral site drainage cannula) configuration. A dedicated, multidisciplinary ECMO team, including a cardiothoracic surgeon, intensivists, a pulmonologist, perfusionists, a respiratory therapist, a nutritionist and ECMO specialist nurses provided care.
We sought to limit sedation, provide an ultra-lung protective strategy (< 4 ml/kg ideal body weight), address delirium and optimize antibiotic therapy and bronchopulmonary hygiene, all in order to allow for lung recovery while the ECMO circuit managed gas exchange. Vascular access was transitioned to a single-site, dual-lumen subclavian catheter on day five in order to facilitate mobilization and physical therapy.
Advertisement
Over the next two weeks, the patient’s condition improved with tailored antibiotic therapy and supportive care. She was separated from VV-ECMO support and decannulated after 14 days. She was liberated from the ventilator four days post decannulation and eventually transferred to the inpatient pulmonary service. She was discharged after 26 days of hospital admission.
At the time of discharge, the patient was on room air and ambulating independently with normal kidney functions and a normal echocardiogram. At her follow-up in the outpatient post-ECMO clinic six weeks later, she was back to her usual state of health. Chest CT revealed near total resolution of the consolidation and cavities. Six-minute walk and pulmonary functions tests, as well as psychological, social and nutritional assessment scores, were within normal limits.
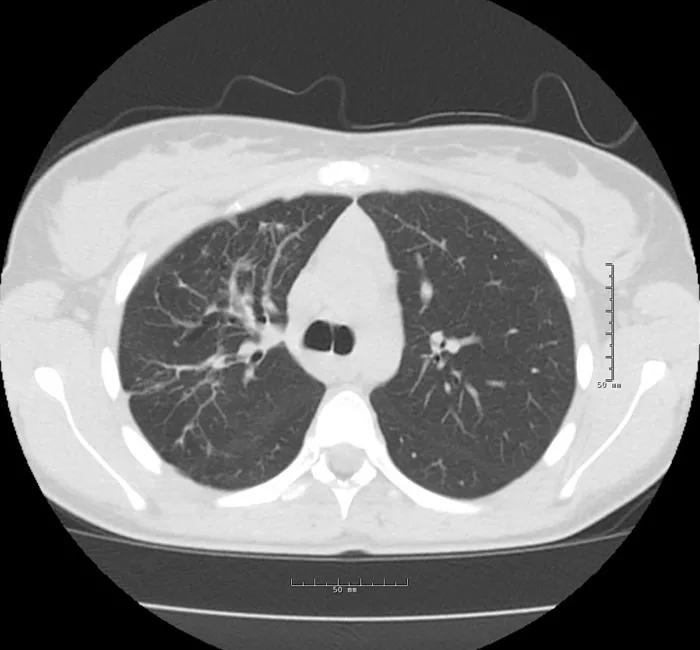
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b8cfe3a3-ae0d-4bee-8e7a-b7b512f41f17/18-PUL-4873-Krishnan-Inset-Image-02-650pxl-width_jpg)
CT scan at outpatient follow-up, six weeks after hospital discharge.
The positive outcome in this challenging case is a testament to the close collaboration amongst a multidisciplinary group of caregivers and the specialized expertise available at Cleveland Clinic.
Dr. Krishnan is staff in Cleveland Clinic’s Department of Critical Care Medicine.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program