Superiority continues even after significant crossovers from control group at 2 years
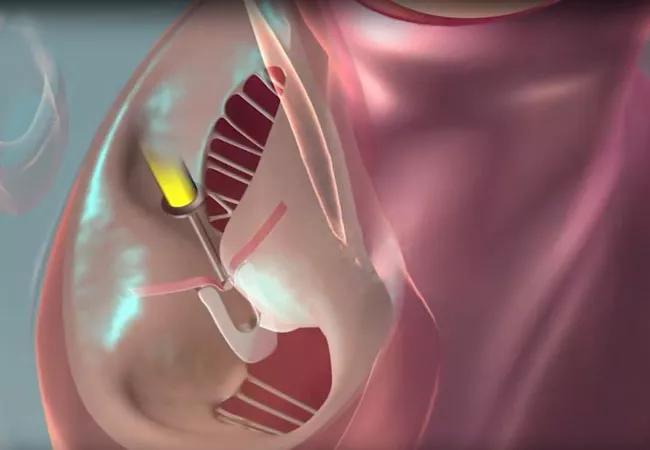
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/673123f4-935e-4a29-a68d-591bb924c3a3/23-HVI-3606658_mitraclip_650x450_jpg)
23-HVI-3606658_mitraclip_650x450
Outcome benefits from transcatheter edge-to-edge repair (TEER) of the mitral valve endure through five years in patients with heart failure and moderate-to-severe or severe secondary mitral regurgitation (MR) who remain symptomatic despite guideline-directed medical therapy, according to final results from the multicenter COAPT randomized trial.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings, which were reported in a late-breaking clinical trial presentation at the American College of Cardiology’s 2023 Scientific Session and simultaneously published online in the New England Journal of Medicine, offer reassurance about the longevity of TEER in this population, says Samir Kapadia, MD, one of the COAPT trial’s lead investigators and a member of its steering committee.
“Given the severity of illness and comorbidities of symptomatic patients with heart failure and significant MR, there was uncertainty about whether the benefits with TEER at two years in the COAPT cohort would remain meaningful out to five years,” says Dr. Kapadia, Chair of Cardiovascular Medicine at Cleveland Clinic. “These are older patients with a very poor prognosis because of concurrent heart failure and valve dysfunction. The message from this trial is that TEER really helps these patients over a number of years.”
“In these patients with functional mitral regurgitation, surgery is often high risk, and TEER demonstrates sustained benefits,” adds A. Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic, who served on advisory and central eligibility committees for the COAPT trial.
Two-year COAPT results were published in 2018 and supported FDA approval of the TEER device used in the trial, MitraClip™, for treatment of symptomatic secondary MR in patients with heart failure.
As reported then, the multicenter, parallel-group, open-label trial randomized 614 patients to TEER with MitraClip plus medical therapy or to medical therapy alone. All patients had heart failure with moderate-to-severe or severe secondary MR and remained symptomatic despite maximally tolerated guideline-directed medical therapy.
Advertisement
At the end of two-year follow-up, patients in the control group who still met the study’s original enrollment criteria were allowed to cross over to TEER with MitraClip. Overall, 67 patients in the control group (21.5%) ultimately underwent TEER — five before two years and 62 after two years — representing nearly half (44.9%) of control group patients who survived to two years.
Five-year follow-up was completed in 89.4% of patients in the device group and 84.6% of those in the control group. Key outcomes at five years included the following, with outcomes in the control group including those who crossed over to TEER:
Advertisement
Most of the benefit from TEER was realized within the first three years after randomization. The investigators attribute this chiefly to the study’s crossover design. “The diminished treatment effect during late follow-up in this trial was in large part due to the performance of transcatheter edge-to-edge repair in 44.9% of control group patients surviving to 2 years,” the authors write in their study report.
Among control patients who crossed over to device therapy, MR reduction and event rates after TEER were similar to those in patients initially assigned to the device group.
“Despite protocol-permitted crossover treatment after two years in the control group, outcomes within the group randomized to TEER maintained clear statistical superiority through five years,” Dr. Kapadia observes. He says this confirms the pathophysiologic proposition behind the COAPT trial — namely, the concept that treating the consequence of cardiomyopathy in this population (i.e., MR due to impaired coaptation of the mitral leaflets), rather than the cause of the disease, can yield a lasting positive impact on heart function, likely because it prevents further deterioration of cardiomyopathy from volume overload.
The investigators note that although death or hospitalization for heart failure had occurred by five years in significantly fewer patients in the device group than in the control group (73.6% vs. 91.5%; HR = 0.53 [95% CI, 0.44-0.64]), the rate was soberingly high even in the TEER-treated patients.
Advertisement
“Adverse events continue to accrue in this high-risk population, even with valve repair,” says Amar Krishnaswamy, MD, Section Head of Invasive and Interventional Cardiology at Cleveland Clinic and a participating clinician in the trial. “These event rates underscore the need for additional therapies to mitigate the underlying left ventricular dysfunction in this population, including close follow-up and optimization of guideline-directed medical therapies by trained heart failure specialists.”
The fact that almost half of control group patients died before they gained eligibility for treatment crossover at two years further illustrates the severity of illness in this population, Dr. Krishnaswamy adds. “This argues for early identification and swift treatment of heart failure patients in whom TEER is appropriate,” he says.
Dr. Kapadia agrees that these positive final COAPT results will increase use of TEER in this population. “They will also fuel interest in new studies of TEER in patients at earlier stages of MR, such as moderate MR,” he says.
The COAPT trial was sponsored and funded by Abbott, which markets MitraClip.
Advertisement
Advertisement
Scenarios where experience-based management nuance can matter most
Optimal management requires an experienced center
Multimodal evaluations reveal more anatomic details to inform treatment
Provides option for patients previously deemed anatomically unsuitable
While mortality was unaffected, later surgery was associated with more reoperations
Surgical tips on debridement of calcification to optimize valve replacement
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon