Patient series and bench validation support efficacy and safety of CLEVE procedure
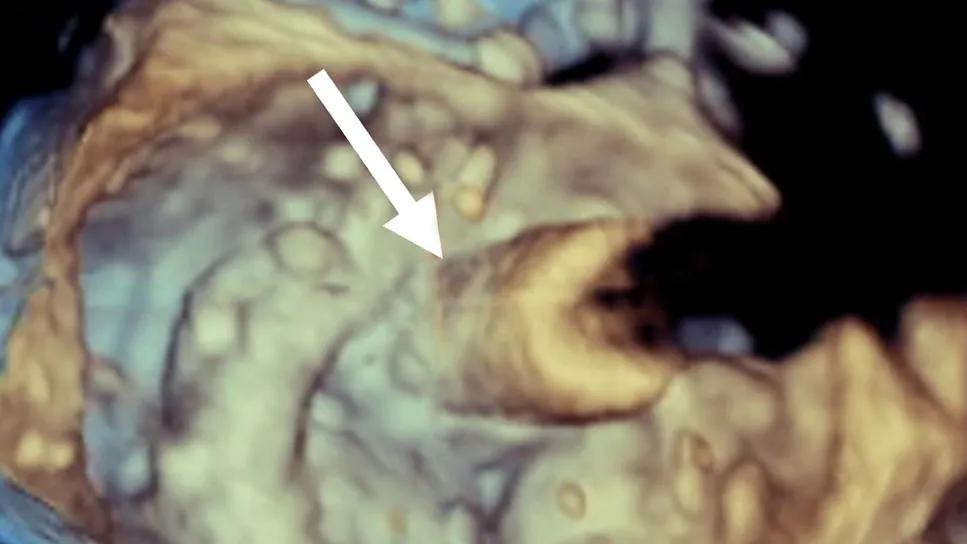
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/86b144da-49ba-4757-8374-f5ced6dad783/CLEVE-figure-cardiac-consult-feature)
3D echocardiogram from a heart valve procedure
A novel Cleveland Clinic-developed procedure for transcatheter valve-in-valve (ViV) replacement of degenerated surgical aortic and mitral valves has moved one step closer to fulfilling its potential as a safe, efficacious treatment for patients who require prosthetic leaflet modification.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The CLEVE (CLEveland Valve Electrosurgery) procedure employs a pioneering electrosurgical technique to lacerate the surgical valve leaflet in a manner that frees it from the surgical valve frame. This prevents its displacement to the periphery of the surgical frame, where it may obstruct the ostial coronary arteries or left ventricular outflow tract.
An early use of the CLEVE procedure for ViV transcatheter mitral valve replacement (TMVR) was published as a case report in late 2023, although the Cleveland Clinic group had been using the procedure as early as 2021 to facilitate ViV transcatheter aortic valve replacement (TAVR) inside a degenerated TAVR prosthesis and in numerous cases involving the mitral and aortic positions since then. A review of Cleveland Clinic’s entire clinical experience with CLEVE — along with results of bench validation — has just been published in JACC: Cardiovascular Interventions (2025;18[6]:767-781) and confirms complete clearance of the offending leaflet in 100% of cases.
“We’ve been performing this procedure since 2021 and have been rigorous in reviewing each case to understand how to optimize the technique,” says the new paper’s lead author, Amar Krishnaswamy, MD, Section Head of Invasive and Interventional Cardiology. “It’s exciting that we are able to move this approach forward and offer transcatheter solutions to patients who previously had no option at all or would have to undergo a high-risk redo cardiac surgery.”
Although the vast majority of patients with failing aortic or mitral surgical prostheses can undergo traditional transcatheter ViV replacement, a small number require leaflet modification. Two procedures have traditionally been used for this purpose: BASILICA (Bioprosthetic or native Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction during TAVR) and LAMPOON (Intentional Laceration of the Anterior Mitral leaflet to prevent left ventricular outflow obstruction during TMVR). Both were pioneered by investigators outside of Cleveland Clinic and have been used worldwide in hundreds of patients.
Advertisement
Drawing on their high-volume experience in TMVR and TAVR, Cleveland Clinic interventionalists — led by Dr. Krishnaswamy and Samir Kapadia, MD, Chair of Cardiovascular Medicine — suspected that the options for leaflet modification could be expanded and perhaps improved through the use of transcatheter electrosurgery. This emerging field — pioneered by interventional cardiologists and cardiovascular imaging specialists at the National Institutes of Health and Washington Hospital Center in Washington, D.C, Emory University in Atlanta, and the University of Washington in Seattle — focuses on the application of radiofrequency energy to wires inside the body to lacerate various anatomic structures.

Image content: This image is available to view online.
View image online ( https://assets.clevelandclinic.org/transform/dc4314e0-f204-450c-96ed-86757e998188/CLEVE-figure-cardiac-consult)
CLEVE procedure to facilitate mitral ViV replacement. (A) A catheter and wire (arrow) are used to perforate the base of the surgical valve leaflet followed by (B and C) inflation of a balloon in the leaflet (arrows) to (D) begin to separate the surgical leaflet from the valve frame (arrow). (E and F) The valve is then positioned through the perforation/hole and deployed in place as shown in panel G. (H) Flow from the left ventricle (LV) passes to the aorta (Ao) unimpeded by the surgical valve leaflet overhanging the open stent struts of the new valve (arrow).
In their new research paper, Drs. Krishnaswamy and Kapadia and Cleveland Clinic colleagues reported on results with the electrosurgery-based CLEVE procedure in their initial 14 patients. All patients had degenerated surgical valve prostheses — eight in the aortic position and six in the mitral position — and were at high risk for obstruction of the left main coronary artery (TAVR) or the left ventricular outflow tract (TMVR).
Successful leaflet clearance was obtained in all 14 cases without obstruction of the ostial coronary artery or the left ventricular outflow tract. Left main trunk obstruction occurred in one patient as a result of suspected embolization of leaflet calcium and/or leaflet material that was noted after ViV deployment. No other complications occurred through 30 days across the series.
Advertisement
To ensure that the CLEVE technique would be safe as well as effective, Drs. Krishnaswamy and Kapadia partnered with Stephanie Sellers, PhD, MSc, and her team in the respected translational research lab at St. Paul’s Hospital in Vancouver, British Columbia, Canada.
“Their benchtop analyses were helpful in demonstrating that in either the aortic or the mitral position, we were fully eviscerating the surgical leaflet from the surgical annulus in the area of potential complication while the leaflet remained attached at the commissural post,” Dr. Krishnaswamy explains. “That helped allay fears that we would be inadvertently embolizing a large piece of surgical leaflet, which could create complications. Knowing that the leaflet pulls away from the surgical frame but remains attached at the post or posts is an important reassurance.”
The benchtop analyses also revealed some flexibility in the location of leaflet perforation. “They provided confirmation that a slight variability in location would produce the same or similar results,” Dr. Krishnaswamy adds.
How does CLEVE compare to BASILICA and LAMPOON?
“There are no comparative data to indicate that one approach or the other is better, safer or more effective,” Dr. Krishnaswamy notes. “However, we believe BASILICA and LAMPOON would not have been anatomically suitable for a number of the patients in whom we have performed CLEVE, due to the pattern of leaflet calcification. Over time, as experience grows at our center and others, we hope that a comparative trial or at least a retrospective comparison of outcomes can be undertaken. This would shed light on relative risks and benefits of the procedures and on whether specific cases are better suited to one approach over another.”
Advertisement
“Key potential advantages of the CLEVE procedure are its simplified steps and the certainty of displacing enough leaflet tissue to prevent obstruction, especially when the leaflets are calcified,” Dr. Kapadia notes. “But a potential shortcoming is the possibility of more hemodynamic instability when the leaflets are detached with the balloon compared with other laceration techniques.”
At Cleveland Clinic, the procedure has become a standard technique. “The number of cases in which we have used CLEVE has grown since the series for the JACC: Cardiovascular Interventions paper was completed,” Dr. Krishnaswamy says. “We are now using it almost exclusively rather than the other leaflet modification procedures.”
“Dr. Kapadia and his team have developed a very innovative and novel technique that avoids obstructing the coronary arteries or the blood flow from the heart when placing a percutaneous valve inside a previously replaced valve,” notes cardiothoracic surgeon Nicholas Smedira, MD, MBA. “This is a useful option in patients who are considered too high a risk to undergo a repeat operation.”
Advertisement
Advertisement
TVT Registry analysis could expand indication to lower surgical risk levels
In the wake of NOTION-3 findings, a strong argument for physician judgment remains
Post hoc analysis of PROTECTED TAVR finds reduced stroke risk in the U.S. but not beyond
Analysis of STS/ACC TVT Registry finds greatest benefit in patients with prior stroke
TAVR explant demands multidisciplinary expertise
How our HVTI Advisory Services team facilitated swift improvements for an allied health organization
Support for a TAVR-first approach in patients with concurrent valve and coronary disease
Five-year data demonstrate convergence of outcomes from years 1 to 5