Combination therapy demonstrates effectiveness in first-line treatment setting

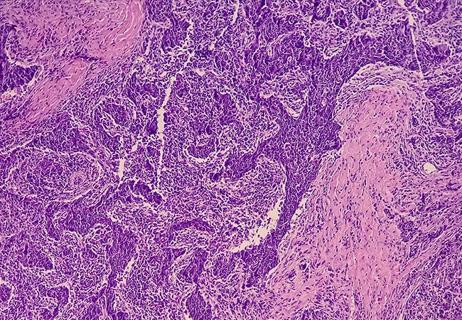
BCA101, a first-in-class bifunctional inhibitor of epidermal growth factor receptor (EGFR) and transforming growth factor beta (TGF-β), shows encouraging antitumor activity, especially when combined with the immune checkpoint inhibitor pembrolizumab, and is well tolerated as first-line therapy in patients with recurrent, metastatic head and neck squamous cell carcinoma (SCC).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An interim analysis of an open-label dose expansion cohort of a phase 1 study showed an overall response rate of 48% and a clinical benefit rate of 74% with the combination of BCA101 and pembrolizumab in a first-line setting in 31 evaluable patients with recurrent, metastatic head and neck SCC. Among patients whose tumors were negative for HPV, reflecting a more aggressive disease course, the ORR was 65%.
The data were presented at the 2023 American Society of Clinical Oncology (ASCO) annual meeting. Emrullah Yilmaz, MD, PhD, Associate Director of Precision Oncology at Cleveland Clinic is coinvestigator in the study and co-author of the abstract. Cleveland Clinic continues to enroll patients into further dose expansion cohorts.
“Pembrolizumab has been used for the treatment of recurrent metastatic head and neck cancer in the front line,” Dr. Yilmaz says. “The use of immunotherapy depends on the expression level of the biomarker PD-L1. If PD-L1 is positive, then pembrolizumab alone can be used but response rates to pembrolizumab monotherapy are limited, so it is often combined with chemotherapy, which improves the initial response.”
The problem is that toxicity prevents long-term use of chemotherapy, so responses are not durable. “That’s why we need better strategies to improve the effectiveness of the immunotherapy—we would like more durable responses,” he says.
BCA101 is bifunctional EGFR antibody fused to a TGF-β immune modulating payload, which has demonstrated clinical activity as monotherapy. EGFR is a well-known target for head and neck cancer, he said. Cetuximab is an EGFR-targeting antibody currently used in this setting but it has limited efficacy as a single agent. “We would expect a stronger response to BCA101 because it also targets TGF-β, and TGF-β is commonly expressed in head and neck cancers and can lead to an immunosuppressive tumor microenvironment,” Dr. Yilmaz says. “This explains the potential that targeting TGF-β along with EGFR might enhance the effectiveness of an immune checkpoint inhibitor.”
Advertisement
The safety of the combination in treating recurrent metastatic head and neck SCC was established in a prior dose escalation cohort of subjects with EGFR-driven advanced solid tumors refractory to standard of care, which determined a tolerable dose with promising clinical activity to be 1,500 mg of BCA101 intravenously given on days 1, 8 and 15, with pembrolizumab given at 200 mg intravenously on day 1, every 21 days. A total of 33 patients with recurrent metastatic head and neck SCC with a PD-L1 combined positive score ≥1 have been enrolled in the single-arm dose expansion cohort, 31 of whom had restaging scans and thus were evaluable. Eligible patients could not have received prior systemic therapy for recurrent or metastatic disease.
The most common primary subsites in the dose expansion study were oropharynx (n=19; 58%), twelve of which were HPV/p16-positive, and oral cavity (n=10; 30%). Twenty-five (76%) patients had distant metastatic disease. While the median progression-free survival in HPV-negative subjects has not been reached, 7 patients have ongoing responses with at least 6.6 months of progression-free survival.
In the HPV-negative subset, the best response was partial response in seven patients and stable disease in three. In the HPV-positive group, there was one partial response and one patient with stable disease as best response.
Twenty-four (73%) patients developed acneiform rash, which is a well-known side effect from EGFR-based treatment and is easily managed. Two patients had grade 3 acneiform rash, and the remaining 22 had grade 1 or grade 2 rash. Three patients (9%) discontinued treatment due to grade 3 or 4 toxicities.
Advertisement
Whether the combination remains tolerable over the long term and whether responses are maintained remain to be determined. “The responses observed in HPV-negative patients are promising and it will be encouraging if patients can tolerate this combination for an extended time,” says Dr. Yilmaz.
Advertisement
Advertisement
Recommendations focus on selecting the right biomarkers for the right setting

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Why Cleveland Clinic is launching its cardioimmunology center

Collaborative patient care, advanced imaging techniques support safer immunotherapy management

Pembrolizumab does not improve outcomes, but immunotherapy may still offer benefit

Highly personalized treatment shrinks tumors resistant to immunotherapy