Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs
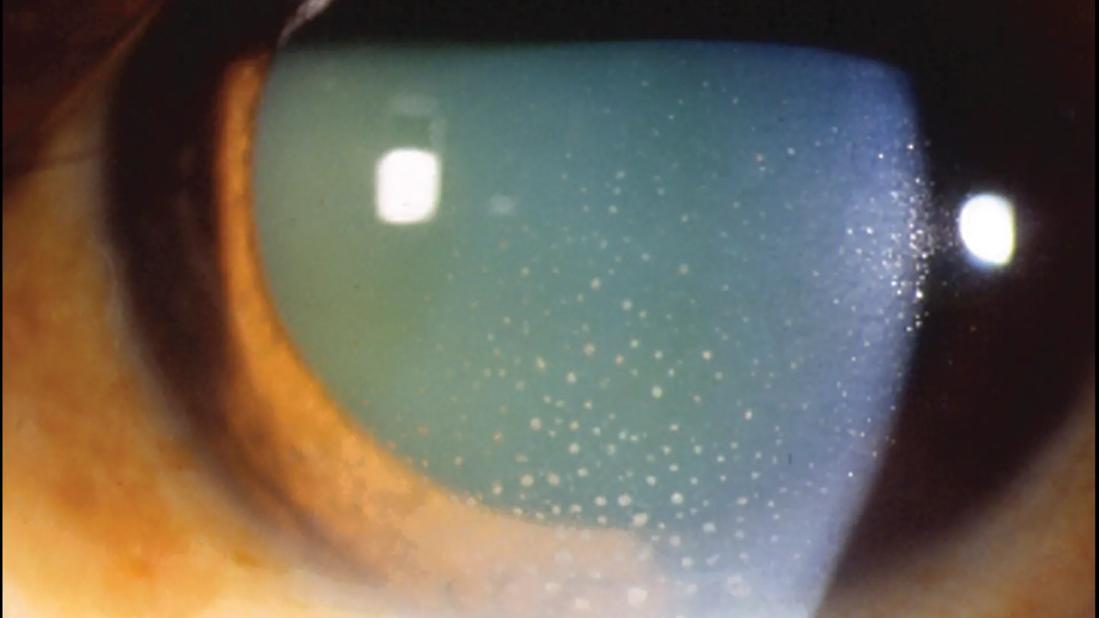
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/45fe8a76-b0d1-4406-8eed-43930e5cd5c2/uveitis)
Eye with uveitis
Patients taking glucagon-like peptide-1 (GLP-1) receptor agonists, commonly used to treat Type 2 diabetes and obesity, have a significantly lower risk of developing noninfectious uveitis compared with patients not taking the medication. This protective effect was found across subgroups of patients with and without diabetes and across different subtypes of noninfectious uveitis, according to a study published in JAMA Ophthalmology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This is the first study to evaluate and demonstrate a possible protective association between GLP-1 therapy and risk of uveitis,” says senior author Sumit Sharma, MD, a vitreoretinal surgeon and uveitis specialist at Cleveland Clinic Cole Eye Institute. “It’s also the first to show a reduction in autoimmune disease with GLP-1 meds.”
Noninfectious uveitis is often associated with autoimmune disease, such as sarcoidosis, juvenile idiopathic arthritis and ankylosing spondylitis. Idiopathic uveitis also typically has autoimmune underpinnings.
Currently there is no preventive therapy for noninfectious uveitis. Primary treatments are short-term steroid therapy for acute flare-ups and long-term immunosuppression for recurring disease.
In addition to helping control diabetes and stimulate weight loss, GLP-1 receptor agonists are believed to have anti-inflammatory properties. A growing body of literature shows that when GLP-1 receptor agonists are administered, there are decreased levels of pro-inflammatory cytokines that are normally seen in the pathogenesis of many inflammatory diseases.
“We were interested in studying the effect of GLP-1 receptor agonists in uveitis, which is fundamentally an inflammatory eye disease,” says Nitesh Mohan, a student at Cleveland Clinic Lerner College of Medicine who was lead author of the study. “Other studies have found that GLP-1 medications are associated with beneficial effects in age-related macular degeneration and glaucoma.
In the JAMA Ophthalmology study, researchers included records of more than 510,000 patients in a national database, about half who were prescribed GLP-1 medication and half who were not. Both groups had a mean age of 56 and were nearly 62% female.
Advertisement
Patients taking GLP-1 receptor agonists had a 51.7% reduced risk of developing new-onset noninfectious uveitis (RR 0.48, 95% CI 0.46-0.51, P < .001). The reduced risk was consistent when studying only patients with Type 2 diabetes (RR 0.54) or patients without diabetes (RR 0.52).
Among patients with diabetes, the risk was about 42% lower in those taking GLP-1 medications compared with those taking metformin or insulin.
“We expected to see that outcome since metformin and insulin aren’t thought to have anti-inflammatory properties,” Mohan says. “SGLT2 [sodium-glucose cotransporter 2] inhibitors initially seemed to be linked with an even lower risk of uveitis compared to GLP-1 receptor agonists, but after doing a sensitivity analysis of patients on monotherapy, we no longer found that association. We are more confident of the decreased risk in GLP-1 medications compared to metformin and insulin.”
Because this was a retrospective, large database study, it relied on accurate ICD coding by clinicians, notes Dr. Sharma. As such, while the magnitude of the relationship between uveitis and GLP-1 receptor agonists was significant, causality is still undetermined.
“Our work was more of a fact-finding project,” he says. “Our findings make sense from a theoretical standpoint, since GLP-1 medications do have an anti-inflammatory mechanism, but we can’t guarantee the association with uveitis.”
More research with different methodologies, such as retrospective chart reviews and prospective trials, is needed to confirm the findings and inform clinical practice. Still, this early study indicates GLP-1 medications’ therapeutic potential in ocular inflammatory disease.
Advertisement
“Certain populations are at increased risk of uveitis: people with a family history of uveitis, people with a genetic predisposition to uveitis and people with autoimmune disease,” Mohan says. “So, for these patients, if there are indications for a diabetes or weight loss medication, it may make sense to prescribe a GLP-1 receptor agonist.”
Advertisement
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
Registry data highlight visual gains in patients with legal blindness
It’s the first step toward reliable screening with your smartphone
Fixational eye movement is similar in left and right eyes of people with normal vision
Oral medication may have potential to preserve vision and shrink tumors prior to surgery or radiation
A new online calculator can determine probability of melanoma
Only 33% of patients have long-term improvement after treatment
Novel collaborative approach helps patient avoid orbital exenteration