Why we favor a tailored approach to relieve LVOT obstruction
For most cases of symptomatic hypertrophic cardiomyopathy (HCM), septal myectomy is adequate to relieve left ventricular outflow tract (LVOT) obstruction. However, some patients have other anomalies causing LVOT obstruction, with or without septal hypertrophy, necessitating a more personalized strategy to address the problem.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Obstructive hypertrophic cardiomyopathy is a very heterogeneous disease with a varied phenotype,” says Milind Desai, MD, MBA, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center. “An individualized treatment plan, informed by thorough evaluation with multimodality imaging and multidisciplinary collaboration, is essential for achieving optimal outcomes.”
Dr. Desai urges that patients diagnosed with or suspected of having HCM be referred to a center with expertise in the condition. While classic cases may be easy to recognize (i.e., patients with a characteristic provokable gradient and thick basal septum), some patients lack significant septal hypertrophy but still have LVOT obstruction, which still puts them at risk for progression to severe heart failure and sudden death.
Maximum LVOT pressure gradient is assessed at rest and with provocation. Any and all means should be used to provoke an LVOT gradient in a symptomatic patient, including amyl nitrite, the Valsalva maneuver and treadmill/bicycle testing, as clinically indicated.
“Determining that someone does not have HCM based on lack of left ventricular hypertrophy is not appropriate,” says Dr. Desai. “Furthermore, diagnosing someone with nonobstructive HCM without the full extent of provocation is also inappropriate.”
Patients should be evaluated with transthoracic echocardiography and cardiac magnetic resonance imaging, with special attention to the following features:
Advertisement
A Cleveland Clinic series of 121 patients with HCM and LVOT obstruction but without basal septal hypertrophy published in 2015 in Circulation: Cardiovascular Imaging found that abnormalities of the mitral valve, chordae and papillary muscles were associated with LVOT obstruction and that procedures to correct these problems, with or without myectomy, may be of benefit.
Nicholas Smedira, MD, MBA, Surgical Director of the Hypertrophic Cardiomyopathy Center, has extensive experience with complex HCM, having operated on about 2,500 cases. He notes that even with that experience, surgeries on these patients continue to pose new challenges.
“One size does not fit all,” he says. “In many cases, you need to be creative.”
A mitral valve or below-valve intervention is often combined with myectomy in patients with LVOT and only moderate septal hypertrophy. Procedures may include:
Advertisement
“These interventions can be safely undertaken with long-term relief of LVOT obstruction when performed by an experienced surgeon in a high-volume, specialized center,” says Dr. Smedira.
He cites a 2019 article in the Journal of Thoracic and Cardiovascular Surgery analyzing over 1,500 operations performed at Cleveland Clinic between 2005 and 2015 for LVOT obstruction, about one quarter of which were myectomies combined with a mitral valve or subvalvular apparatus intervention. Overall, in-hospital permanent pacemaker insertion was needed in 5.3% and operative mortality was 0.38%.
When a mitral valve procedure is required, repair is preferred over replacement. If repair is not possible, however, Dr. Smedira performs careful placement of a biological valve, ensuring that struts do not protrude and cause obstruction, avoiding the need for lifelong warfarin with a mechanical valve.
Dr. Desai notes that a recent Cleveland Clinic study (J Am Heart Assoc. 2021;10:e016210) of 2,268 patients with obstructive HCM undergoing either a myectomy or any of the additional procedures described above found that there is no outcome penalty for performing these procedures along with myectomy. “The long-term outcomes of these patients were similar to those of the age- and sex-matched general population,” he says.
For patients who cannot tolerate or are refractory to medical therapy but are not candidates for open-heart surgery, two catheter-based options — one old and one new — can relieve LVOT obstruction.
Advertisement
Alcohol septal ablation, first introduced in the mid-1990s, involves injecting a small amount of alcohol percutaneously into one or more arteries supplying the septum. This induces myocardial necrosis, with subsequent scarring and widening of the LVOT. The procedure is associated with symptomatic improvement and good long-term survival, but it may induce arrhythmias requiring a pacemaker.
“Although alcohol ablation is now performed in many centers, experience is critical so that it is done in appropriate patients in an appropriate way,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic. “It is important to understand a patient’s anatomy and options before committing the patient to alcohol ablation. For this reason, a heart team approach — with HCM expert clinicians, surgeons and interventional cardiologists — is essential for selecting appropriate candidates for alcohol ablation.”
The MitraClipTM is designed to address primary mitral regurgitation and has started to be used in HCM. The percutaneous device grasps and coapts the mitral valve leaflets, accomplishing a tailored repair. Dr. Desai notes that further data on its use in this setting will be forthcoming.
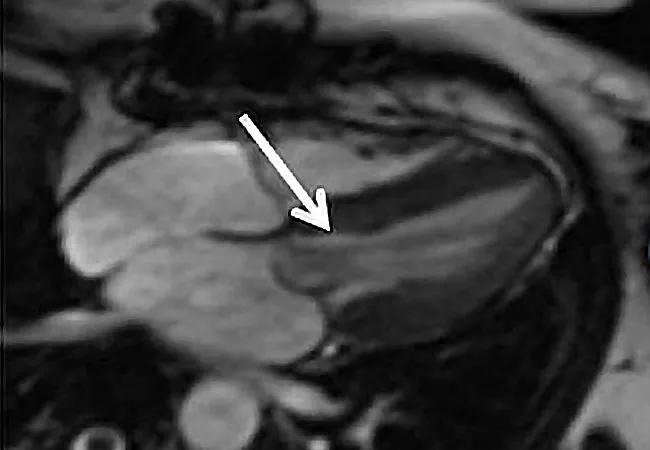
Image at top: Cardiac MRI showing one manifestation of atypical LVOT obstruction, abnormal chordal attachment (arrow).
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more