Program expands as data continues to show improved outcomes

Postoperative health status, body image satisfaction and quality of life rebound to preoperative levels quickly in donors undergoing laparoscopic donor hepatectomy (LDH) for living donor liver transplantation, according to a recent study published in Annals of Transplantation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Choon Hyuck David Kwon, MD, PhD, coauthored the prospective, single-center study, which began when he led the program at South Korea’s Samsung Medical Center before becoming Cleveland Clinic’s Director of Laparoscopic Liver Surgery.
“Quality of life is really important in what we do, because our donors are healthy people who are volunteering for the surgery,” says Dr. Kwon. “Returning to their previous health status after surgery is perhaps even more important to a donor than it might be to a transplant recipient who also wants to fully recover but ultimately needs a procedure to survive.”
Dr. Kwon notes that although the open donor hepatectomy (ODH) control group in the study was small (N = 2), the significant postoperative differences observed in LDH patients (N = 45) versus ODH patients are consistent with findings from other studies. The special ethical considerations of living donor surgery precluded group randomization, and most enrollees in the study opted for laparoscopic surgery, meaning nonparametric statistical methods were needed to compare the ODH and LDH groups. The Samsung program moved exclusively to LDH soon after the research began.
The researchers surveyed patients for health status assessment and quality of life (QOL) on the day prior to operation, during hospitalization, on their discharge date and then at 1, 6 and 12 months postoperatively using the Enhanced Recovery After Surgery Mobility Scale (EMS), the Body Image Questionnaire (BIQ) and the Eq-5D®, a generic health-related QOL questionnaire.
Advertisement
Patients in the LDH group were independently mobile from postoperative day 5, earlier than the ODH patients. The LDH group had significantly higher mean EMS scores than the ODH group on postoperative days 5 and 7 (P = 0.011 and P = 0.004, respectively). Body image scores for the LDH group were significantly higher than that of the ODH cohort at 1 month (P = 0.017). QOL in the LDH group returned to preoperative values at 6 months (P = 0.059) and 1 month (P = 0.217), respectively. “We now have further evidence that laparoscopic is a superior approach in terms of donor recovery,” says Dr. Kwon.
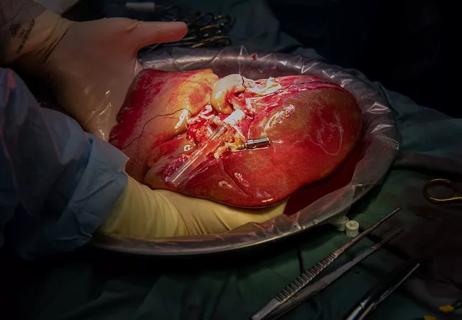
While LLDH can help increase the supply of donor livers, the procedure is technically demanding and complex. Its use is mostly confined to Asia and is not widely practiced in the U.S.; Cleveland Clinic’s LDH program is the nation’s most active and the only U.S. program to use the laparoscopic approach for all living donors. Dr. Kwon founded the program at Samsung Medical Center in 2013 before being recruited to Cleveland Clinic in 2018 to begin the nation’s second LDH program.
“As of November 2022, we’ve completed over 90 procedures and have been the only fully laparoscopic program in the U.S. since 2019,” says Dr. Kwon.
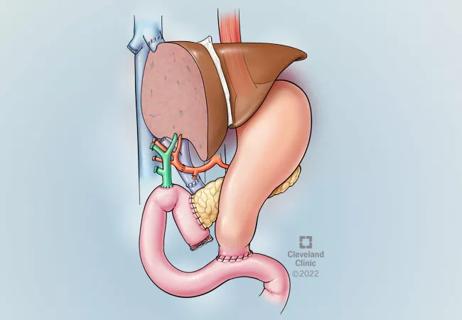
While globally, 95% of LDH resections involve the right lobe of the liver, Cleveland Clinic’s program now has more left lobe donors than right.
“Working with the Director of Living Donor Liver Transplant, Koji Hashimoto, MD, PhD, we’ve determined when modification of portal venous flow is needed to alleviate the risk of overflow injuries that result in small-for-size syndrome,” Dr. Kwon says. “It enables us to use grafts as small as 35% of standard liver volume and yet have very good outcomes. Our donors recover so much better, and I think left lobe donations will be the trend in the coming decade.”
Advertisement
Dr. Kwon and colleagues are preparing a manuscript detailing their experiences at Cleveland Clinic to share best practices for building a safe, robust laparoscopic living donor program that will help address a paucity of data specific to populations in the West.
The program also recently hired Jaekeun Kim, MD, a leading expert in robotically assisted liver resection, to expand the program to include robotically assisted living donor hepatectomy, which Dr. Kwon believes other surgeons could adopt more readily. “Laparoscopic living donor hepatectomy has a bit steeper learning curve,” he says, “and the robotically assisted program could allow us to eventually make this procedure more accessible to more surgeons as part of our educational mission.”
Advertisement
Advertisement

Enhanced visualization and dexterity enable safer, more precise procedures and lead to better patient outcomes

Minimally invasive approach, peri- and postoperative protocols reduce risk and recovery time for these rare, magnanimous two-time donors

Patient receives liver transplant and a new lease on life

New research shows dramatic reduction in waitlist times with new technology

Cleveland Clinic study shows positive outcomes for donors and recipients

Program's approach maximizes donor safety without compromising recipients' outcomes
Atypical cells discovered after primary sclerosing cholangitis diagnosis
Research examines risk factors for mortality