Cleveland Clinic study shows positive outcomes for donors and recipients

Laparoscopic living donor hepatectomy (LDH) with a left-lobe graft (LLG) for living donor liver transplantation (LDLT) is beneficial for both donors and recipients, according to Cleveland Clinic’s first comprehensive study of its LDLT program which was presented at the annual meeting of the American Surgical Association.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To provide the best possible outcomes for donors, Cleveland Clinic has embraced the latest advances in living donor liver transplantation – LLG and laparoscopic LDH. In 2019, the LDLT program instituted a laparoscopic LDH program, the first in the Midwest and second in the United States. Since then, all donor hepatectomies have been performed laparoscopically, making it the most active program in the U.S.
Laparoscopic LDLT is a highly complex procedure requiring specialized expertise and equipment. It is most commonly used in Asia. While laparoscopic LDH reduces the risks associated with open LDH, such as infection, adhesion and hernia, the use of laparoscopic instruments allows less room to maneuver, which creates challenges for spatial orientation during blood vessel and bile duct dissection and for rapid response in the event of hemorrhage or other complications.
Surgeons need expertise in both living donor liver transplantation and experience in advanced laparoscopic technique. The liver transplant surgical team had intensive training under the supervision of the Director of Laparoscopic Liver Surgery Choon Hyuck David Kwon, MD, PhD, who was recruited to Cleveland Clinic from South Korea’s Samsung Medical Center, where he founded the first laparoscopic LDLT program in 2013.
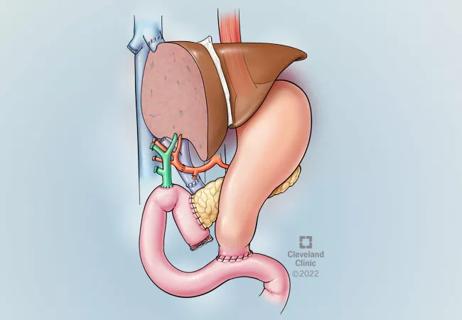
Since 2013, the liver transplant program has followed an LLG-first policy since LLG allows lower morbidity to the donor. LLG is the preferred option when the graft-to-recipient weight ratio (GRWR) is ≥0.6%. Right-lobe grafts are the second choice when the remnant volume is ≥ 30%. The challenge is removing the least amount of liver function in the donor while obtaining a large enough graft to sustain smooth recovery in the recipient. The major risks of LLG for the recipient are liver dysfunction and small-for-size syndrome (SFSS) from using smaller left lobes. But these can be mitigated with the correct surgical technique, both on the donor and recipient.
Advertisement
“When you know how to use a left-lobe graft, you can have good outcomes in the recipient while also protecting the donor. When the donor has a larger percentage of the remaining liver, they have a faster and easier recovery,” says Dr. Kwon.
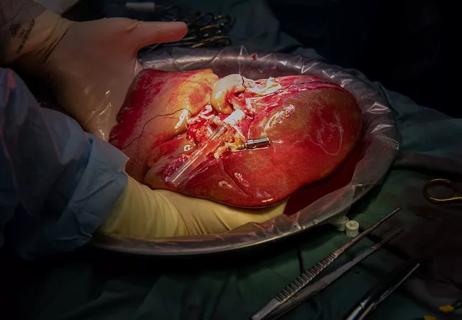
From 2012 to 2022, Clinic transplant surgeons performed 216 LDLTs: 104 laparoscopic and 112 open. The study cohort included 188 cases: 92 laparoscopic and 96 open, after excluding pediatric and right posterior section grafts.
The laparoscopic procedures included 19 grafts with biliary and/or portal vein anatomic variance. Intraoperative conversion to open was needed in only one case with portal vein anatomical variance. The mean operative times were similar in both laparoscopic and open surgeries (368 vs. 359 minutes). Patients who had laparoscopic surgery had a shorter hospital stay, lower blood loss and lower peak AST. They also had a lower 90-day complication rate (41% vs 14%) and a lower rate of late complications such as hernia that required surgery compared to open cases.
Nearly half of the donor surgeries (49%) used a left-lobe graft. Peak bilirubin was lower in LLG donors compared to RLG donors (1.4 mg/dL vs. 2.4 mg/dL) and was lowest in LLG donors with the laparoscopic approach (peak bilirubin, 1.1 vs. 1.6 mg/dL). LLG was also more likely to have a single duct than RLG (88 % vs. 59 %); multiple ducts were avoided in 24 of 91 LDLT procedures (26 %). Obtaining grafts with a single bile duct helps reduce the biliary complication rate on the recipient. Of the LLG procedures, small-for-size syndrome occurred in only one case (0.5%). The one-year graft survival of 92% was achieved without any differences between the type of graft (LLG vs. RLG) or type of surgical approach (laparoscopic vs. open).
Advertisement
This is the first study that showed LDH is protective to the graft which allows wider utilization of smaller graft such as LLG, resulting in non-inferior outcome for recipients that use right lobe grafts: “In laparoscopic surgery, the left lobe is more accessible compared to the right. But interestingly, the laparoscopic approach also prevents graft injury so you obtain a better quality graft,” says Dr. Kwon. “When you get as good outcomes for the recipient, there’s no reason to use the right lobe and risk more complication to the donor.”
This study’s positive outcomes may influence the liver transplant landscape. “Some in the medical community still have reservations about living donor liver transplantation, because of concerns about donor risk. This study affirms that living liver donation is a safe, practical approach that saves lives,” says Dr. Kwon.
As more people learn about the laparoscopic approach “it has the potential to attract more liver donations, as it did for kidney donations,” says Dr. Kwon.
Advertisement
Advertisement

Enhanced visualization and dexterity enable safer, more precise procedures and lead to better patient outcomes

Minimally invasive approach, peri- and postoperative protocols reduce risk and recovery time for these rare, magnanimous two-time donors

Patient receives liver transplant and a new lease on life

New research shows dramatic reduction in waitlist times with new technology

Program's approach maximizes donor safety without compromising recipients' outcomes

Program expands as data continues to show improved outcomes
Atypical cells discovered after primary sclerosing cholangitis diagnosis
Research examines risk factors for mortality