Surgical tips on debridement of calcification to optimize valve replacement
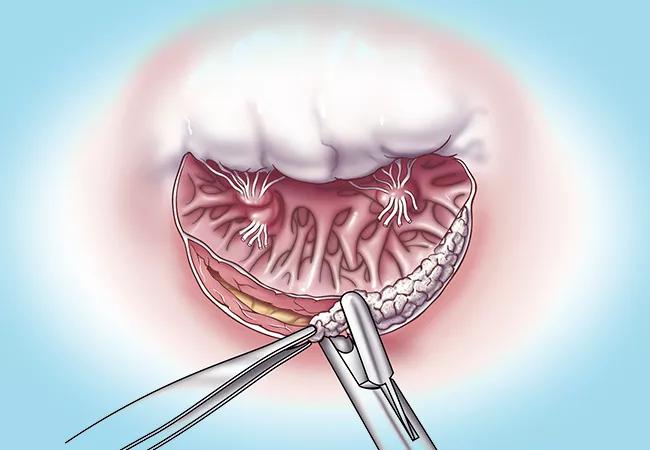
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1a915d8f-24f5-45fe-876f-e0f3554e8977/23-HVI-3655709-CQD-650x450-c2_jpg)
23-HVI-3655709 CQD 650×450-c2
In the setting of mitral annular calcification (MAC) in a patient undergoing mitral valve replacement, addressing the calcium to achieve optimal sizing and seating of a prosthetic valve offers the best chance of favorable results. But special care must be taken to avoid releasing calcium fragments into the bloodstream or injury to the atrioventricular groove or a left circumflex coronary artery; these potential high-risk complications deter most surgeons from adequately addressing MAC.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic cardiothoracic surgeons have considerable experience with careful but sometimes aggressive handling of MAC, prompting an invited talk on the subject by Haytham Elgharably, MD, at the 2023 annual meeting of the Society of Thoracic Surgeons. In addition to discussing MAC assessment and tailoring the surgical approach to MAC severity, Dr. Elgharably provided procedural guidance for safely addressing this difficult situation.
“Removing MAC is technically challenging, but in many cases doing so offers the best outcome by providing a smoother and more pliable surface for implanting an appropriate-size prosthesis that meets the patient’s requirements of adequate blood flow and cardiac output,” Dr. Elgharably says. “With careful attention to presurgical planning and intraoperative technique, it can be done safely at centers of expertise.” Highlights of his presentation are recapped below.
MAC severity must be thoroughly evaluated preoperatively so that the strategy can be individually tailored and planned. A multimodality imaging assessment is recommended, including:
“MAC is a highly heterogeneous disease,” says cardiologist Serge Harb, MD, of Cleveland Clinic’s Section of Cardiovascular Imaging. “It can affect the annulus to varying degrees and may also extend to the mitral leaflets and surrounding myocardial tissue, resulting in various levels of functional impairment. To fully understand the anatomical details and functional implications, a comprehensive preoperative assessment using multimodality imaging is necessary.”
Advertisement
He adds that in certain complex cases, 3D printing of the heart is done based on imaging studies, providing the operator with a realistic model of MAC distribution.
Dr. Elgharably explains that preoperative findings determine the surgical approach. In most cases:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3e794228-3f15-4954-a882-d590b167d2c8/23-HVI-3655709-Inset-2_jpg)
Figure 1. Operative photo showing a Commando exposure. Asc Ao = ascending aorta; LVOT = left ventricular outflow tract; LA = left atrium; RA = right atrium; RV = right ventricle.
Other preoperative planning includes prosthesis type and sizing, taking into account the patient’s body mass, functional status, symptoms, comorbidities and concomitant procedures.
Debridement starts with incising the posterior leaflet to expose the MAC, which is followed by sharp debridement of calcium fragments (Figure 2). After adequate debridement and sizing of the target prosthesis, reconstruction of the posterior annulus is necessary. “The degree of reconstruction required is based on the magnitude of debridement, which depends on the defect size in the annulus, the density of MAC (as determined by tapercut needle if it can go through), the quality of tissues that can be used to support the reconstruction, and the type and size of prosthesis needed,” Dr. Elgharably says.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ebd06f01-6f03-4b1c-a270-4a189b80ac84/23-HVI-3655709-Inset-1_jpg)
Figure 2. Operative photo showing debridement of MAC.
Because the annulus may be weakened as a result, it may need to be reinforced to hold the prosthesis. In general, strategies for reconstruction include the following, according to MAC severity:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7365127b-1a58-4f20-98f4-387a1aeec92d/23-HVI-3655709-Inset-3-1_jpg)
Figure 3. Key steps in the surgical management of severe MAC. (Left) Excision of posterior leaflet that is too calcified to be spared. (Middle) Calcium is debrided with care to avoid injury to the ventricular myocardium and coronary vessels. Calcium fragments must be completely aspirated from the field. (Right) In cases where calcification extends into the atrioventricular groove, a pericardial patch can be sewn on to cover the defect. Valve sutures should pass through the patch and out through the annulus to provide added support.
For the replacement valve, Dr. Elgharably prefers to use a low-profile prosthesis with short struts, as it is easier to seat and avoids obstruction of the left ventricular outflow tract (LVOT).
Dr. Harb says that a well-anchored and optimally positioned prosthetic valve can prevent complications such as paravalvular leaks and LVOT obstruction. The complications can be detected by echocardiography, which he notes is the preferred test for monitoring these patients.
“The margin of error during mitral valve surgery in patients with MAC is small,” Dr. Elgharably concedes. “But as the U.S. patient population ages, MAC is becoming more of a problem, and having the ability to effectively address it grows more important.”
Two detailed overviews of surgical techniques used at Cleveland Clinic to address MAC have been published, one in Operative Techniques in Thoracic and Cardiovascular Surgery (2003;8[1]:2-13) and the other in the Journal of Thoracic and Cardiovascular Surgery (2013;146[1]:233-235).
Advertisement
Advertisement
Scenarios where experience-based management nuance can matter most
Optimal management requires an experienced center
Multimodal evaluations reveal more anatomic details to inform treatment
Provides option for patients previously deemed anatomically unsuitable
While mortality was unaffected, later surgery was associated with more reoperations
Superiority continues even after significant crossovers from control group at 2 years
How Cleveland Clinic is using and testing TMVR systems and approaches
NIH-funded comparative trial will complete enrollment soon