Systemic lupus erythematosus complicates conception, pregnancy
By Lisa Zickuhr, MD, Amanda Kalan, MD, and Howard R. Smith, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 25-year-old African American woman was counselled about contraception. She had a history of systemic lupus erythematosus (SLE), manifesting with arthritis, alopecia, Raynaud phenomenon, leukopenia and lupus nephritis, and her disease was previously well controlled on hydroxychloroquine (HCQ), mycophenolate mofetil (MMF) and prednisone.
She conceived before beginning the discussed contraception, prompting discontinuation of MMF. Her serum antibody testing revealed the presence of anti-Ro (SS-A) and anti-La (SS-B) antibodies. Low-dose aspirin and fetal ultrasonographic monitoring were initiated. At the start of her second trimester, wide-spread lesions of cutaneous lupus erythematosus erupted. They responded to high-dose glucocorticoids and azathioprine, but flared when prednisone was weaned. She also developed thrombocytopenia, proteinuria, elevated liver enzymes and hypertension that raised concern for a lupus flare versus preeclampsia. She was admitted to the obstetrics labor and delivery unit for antenatal monitoring of a high-risk pregnancy.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/64931079-3347-40d9-8477-17c6b20bade1/17-RHE-1227-Smith-Hero-Image-650x450pxl_jpg)
Pregnant abdomen with hypo- and hyperpigmentation indicating healing cutaneous lupus erythematosus.
Compared to healthy women, pregnant SLE patients with active disease and major organ involvement have a higher risk of thrombosis, premature delivery, preeclampsia, eclampsia, pregnancy loss and maternal mortality. In some studies, maternal SLE is also associated with fetal intrauterine growth restriction. Many immunosuppressive agents that could potentially control active lupus are known teratogens.
Advertisement
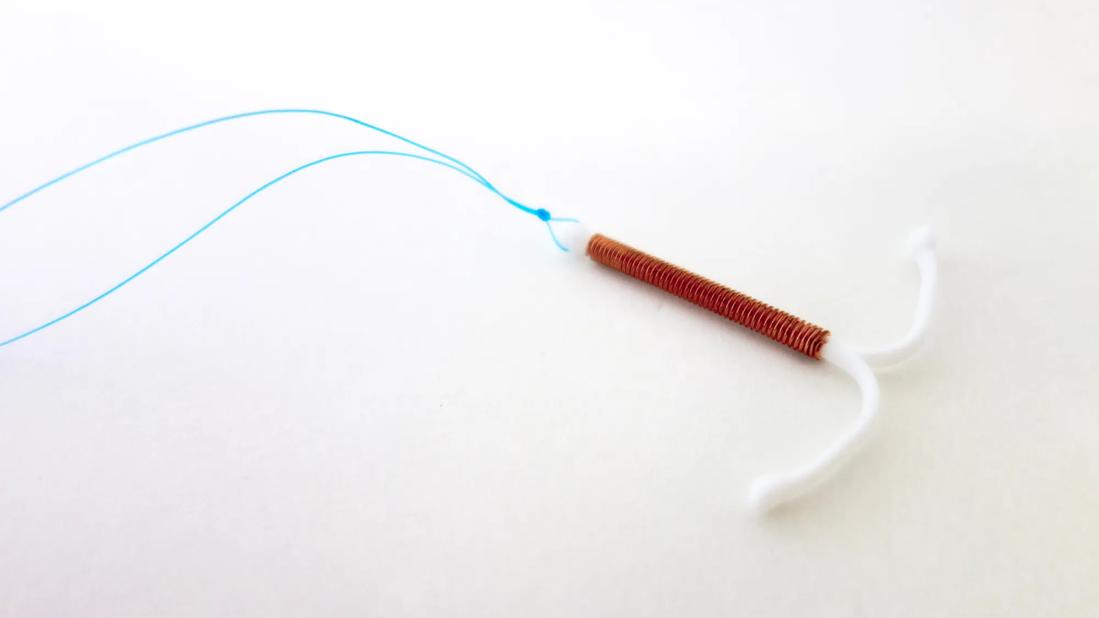
To protect mother and fetus, contraception should be discussed with all female SLE patients, and pregnancies should be planned during inactive disease. Combined hormonal contraception is appropriate for any SLE patient without antiphospholipid syndrome (APS). Those with APS should avoid estrogen-containing products. Copper intrauterine devices offer long-acting, reversible and hormone-free contraception that avoids the thrombotic risks of estrogen.
The rate of SLE flares during pregnancy varies among observational studies but is estimated at 30 to 70 percent. Severe flares can have negative consequences, as active lupus nephritis is a positive predictive factor for poor pregnancy outcomes. Careful, routine monitoring of lupus activity is necessary throughout pregnancy.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eee1f191-9c54-4c67-8c2f-6f125c819204/17-RHE-1227-Smith-Inset-Image-01_jpg)
Bilateral hypo- and hyperpigmentation and erythematous livedo reticularis representing active cutaneous lupus erythematosus.
Rheumatologists and obstetricians play an important role in maternal and fetal monitoring. At risk of preeclampsia and eclampsia, mothers should be monitored for hypertension, thrombocytopenia, proteinuria and swelling. These symptoms characterize preeclampsia and eclampsia, but they can also be seen in SLE flares. Anti-dsDNA antibody and complement levels can help differentiate the two, an important task given the difference in treatments.
We recommend serially checking complete blood cell counts, complete metabolic panels for renal and hepatic function, urinalyses, complement levels and anti-dsDNA antibody levels to monitor SLE activity during pregnancy.
Advertisement
Increased plasma volume during pregnancy can cause dilutional anemia and thrombocytopenia and thus mimic SLE and artificially raise the sedimentation rate. Increased plasma volume also raises the glomerular filtration rate, increasing urine protein and creatinine measurements. As a rule of thumb, 24-hour proteinuria greater than 300mg/dL should be considered pathologic until proven otherwise. Hematuria is abnormal in pregnancy, and lupus nephritis must be ruled out if it is detected. Complement (C3 and C4) levels increase during gestation, as opposed to often decreasing in flares of lupus, but anti-dsDNA antibody levels remain unaffected.
Fetal growth should also be carefully monitored during pregnancy. Additionally, maternal anti-SS-A or anti-SS-B antibodies can cause neonatal lupus, a syndrome characterized by rash, hemolytic anemia, thrombocytopenia and congenital heart block (CHB). Ultrasound surveillance for fetal growth and CHB is common practice. The latter has an incidence of approximately 2 percent in mothers whose previous pregnancies were unaffected by CHB and approximately 15 percent in those affected. Expecting mothers should be treated with glucocorticoids if CHB is detected.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/44fc59d6-462f-4740-aa42-45ea4230a504/17-RHE-1227-Smith-Inset-Image-02_jpg)
Palmar erythema with area of desquamation from active cutaneous lupus erythematosus.
HCQ prevents flares and controls disease activity and can improve outcomes during pregnancy. Low-dose aspirin protects against premature delivery and preeclampsia in healthy pregnant woman and is thus assumed effective in SLE and APS patients.
Advertisement
Glucocorticoids, azathioprine, tacrolimus and cyclophosphamide (after the first trimester, but only in those with severe or life-threatening disease) can be used to treat active lupus during pregnancy. As every medication carries the potential for side effects, disease flares should be treated with agents that have the least potential for causing complications. Intravenous immunoglobulins have been used in refractory cases of SLE in pregnant patients.
Methotrexate, leflunomide, MMF and cyclophosphamide (during the first trimester) should be avoided because of their abortifacient and teratogenic effects. The effects of rituximab and belimumab during pregnancy are not well understood.
The complexity of pregnancy in a patient with SLE clearly warrants management by a multidisciplinary team of expert rheumatologists and obstetricians. The two alone can be complicated, but together they can present a challenge for the clinician, patient and fetus.
Dr. Zickuhr is a fellow in the Department of Rheumatic and Immunologic Diseases. Dr. Kalan is associate staff in the Department of Obstetrics and Gynecology. Dr. Smith is Director of the Lupus Clinic in the Department of Rheumatic and Immunologic Diseases.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment