Case highlights the importance of oral hygiene in hospital and outpatient settings

Note: This article is reprinted from the Cleveland Clinic Journal of Medicine (2023;90[3]:145-146)
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By Sagar Khanna, BDS, DDS
A 60-year-old man was referred by his primary care physician to the oral and maxillofacial surgery clinic with a mass under the upper lip. The mass had grown slowly over the past two to three weeks while the patient was in rehabilitation after a stroke that had occurred three months earlier. He reported no symptoms other than minor bleeding of the gums after brushing his teeth. He was not a smoker. His oral hygiene during his hospitalization and rehabilitation had been poor.
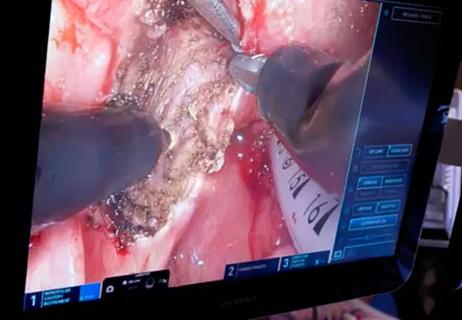
On physical examination, a large, firm, non-tender, sessile mass was visible on the gingiva of the upper incisors (see above). The surface was erythematous and smooth with no ulceration. Excisional biopsy of the entire mass was performed under local anesthesia. Histopathology revealed a fibroma with fibrous strand proliferation and no dysplastic changes, suggesting a diagnosis of benign fibroma. No additional treatment was necessary.
The patient was instructed on the importance of maintaining oral hygiene. At a two-week follow-up visit, the gingiva had healed with restoration of its contour. The patient had no bleeding gums or other symptoms.
The differential diagnosis of a gingival mass includes peripheral ossifying fibroma, peripheral giant cell granuloma and pyogenic granuloma.1 Fibromas are benign growths that occur most commonly along the buccal mucosa secondary to accidental biting of the cheek.2 Due to their slow growth, they typically have a subacute onset.
The gingival fibroma in our patient stemmed from poor oral hygiene resulting in plaque with a calculus deposit acting as an irritant. This is histologically different from a cutaneous fibrous neoplasm, which is rarely seen in the mucosal tissue in the head and neck.3 Excisional biopsy is diagnostic and curative. Laser removal has been described in the literature.4 Recurrence is prevented with attention to good oral hygiene.5
Advertisement
The development of the oral mass in this patient illustrates the importance of oral health, which is often overlooked in the hospital and outpatient settings. Patients at risk include those with prolonged stays in the hospital and in rehabilitation facilities. Patient education and attention to oral hygiene can prevent oral infections and will improve the overall health of patients.
Advertisement
Advertisement
The retrospective study identifies factors that influence disease-free and overall survival

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition