The role of radiologists in preoperative planning and post-uterus transplantation surveillance
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Medical imaging plays a significant role in uterus transplantation, with radiologists performing imaging studies at many points throughout the transplant process, including preoperative imaging of potential recipients and donors, as well as post-transplant surveillance. Although data regarding complications following uterus transplant are preliminary, it is important that we are aware of the risk of vascular compromise and graft failure, and how those complications appear in imaging. As we gain experience with this procedure, it will be important to share what we learn in an effort to establish normal and abnormal imaging criteria and confirm best practices. Together with collaborators from the Cleveland Clinic uterus transplant team, I published an article reviewing uterus transplantation and the role of the imaging throughout the process. This article summarizes the review and offers insight from our initial experience at Cleveland Clinic.
During the selection process, women first undergo imaging — generally ultrasound — to confirm the diagnosis of absolute uterine factor infertility (AUFI). Sometimes women with congenital AUFI may have other renal or vascular anomalies that can impact transplant outcomes. In these cases, CT or MR angiography can aid in presurgical planning. Patients also undergo imaging that is standard for any transplant, such as chest x-rays and, potentially, unenhanced CT if the patient is at risk for atherosclerotic disease.
At Cleveland Clinic, our uterus transplant protocol calls for the use of deceased donors; however, live donors have been used at other sites. Live donors tend to be older and may be at higher risk for atherosclerotic disease. CT of the abdomen and pelvis without contrast is typically performed to evaluate for the presence and extent of vascular calcifications in potential donors at risk for atherosclerotic disease. Some centers use MR or CT angiography to evaluate the uterine vasculature as part of the donor selection process. For both living and deceased donors, the structural integrity of the uterus must be evaluated. Ultrasound is used to look for uterine abnormalities that would render the uterus unsuitable for transplant, such as leiomyomas, congenital malformations, severe adenomyosis or neoplasm.
Advertisement
Currently there is limited information available in the literature about post-uterus transplant imaging. We built our protocol based on our expertise in imaging for other solid organ transplants. We use transabdominal ultrasound with Doppler to evaluate blood flow to, from and within the uterus transplant. These studies are performed daily for the first five days post-transplant and then at routine intervals or when there is clinical concern for a potential problem. Transvaginal ultrasound may also be used after the vaginal anastomosis has healed, usually around eight weeks.
We start with a gray-scale ultrasound of the uterus, endometrium and surrounding tissues. We look for fluid collections or hematomas surrounding the graft which might indicate a problem. We assess the size and echogenicity of the uterus as changes over time could indicate edema or infarction. We also assess the endometrial canal for changes that indicate the onset of the menstrual cycle.
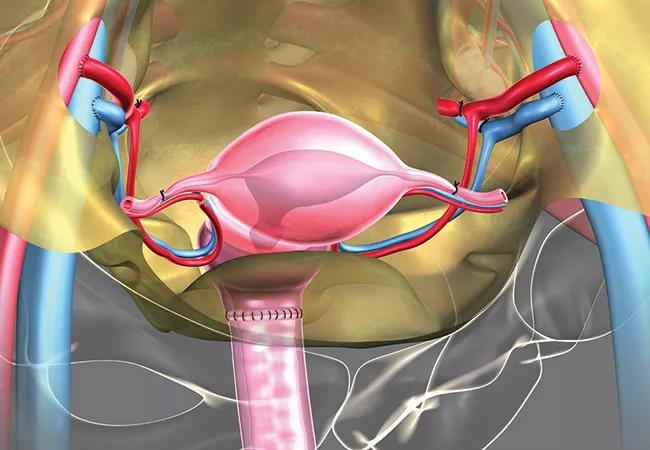
We then use color and spectral Doppler ultrasound to assess the uterus transplant vasculature. We start with color and Power Doppler evaluation of the graft. Here we are checking to see that blood flow can be detected throughout the entire graft and that this flow is symmetric. We then evaluate the arterial supply bilaterally. We carefully evaluate the external iliac artery for patency, ruling out dissection or thrombosis and locate the anastomosis. We follow the uterus transplant artery to the lower uterine segment, looking for patency and signs of stenosis. Finally, we evaluate the intraparenchymal arteries with spectral Doppler. We then turn our attention to the venous outflow. In the venous portion of the exam, we begin by locating the origin of the anastomosis of the external iliac veins and the donor internal iliac vein. In the lower uterine segment, we look for venous flow external to the uterine parenchyma. We also identify intraparenchymal veins and evaluate for patency.
Advertisement
MRI and CT can be used when the ultrasound results are inconclusive; these studies may reveal unexpected postoperative findings, such as infection, hemorrhage, fistula, vascular thrombosis or graft necrosis. The radiologist, transplant surgeons and other physicians on the transplant team are always in close communication to correlate imaging findings with other pieces of clinical information to ensure the best care for our patients.
As early as one to two months following uterus transplantation, the recipient should have her first menstrual period. According to the Cleveland Clinic protocol, embryo transfer can be performed as early as six months after uterus transplantation.
After confirmation of a viable pregnancy, patient care is transferred from the transplant team to a maternal-fetal medicine specialist. Fetal imaging in pregnancy after uterus transplantation follows the same protocol as routine pregnancies, with the addition of serial growth ultrasounds in the late second trimester due to the known risk of fetal growth restriction in patients with other solid organ transplants. In addition, weekly ultrasounds for biophysical profiles are performed after 32 weeks. The biophysical profile is a test that includes assessment of amniotic fluid volume as well as fetal activity and is used to monitor fetal well-being.
At Cleveland Clinic, our protocol allows for up to two babies to be delivered via cesarean section before the transplant is removed delivery and immunosuppressive treatment is stopped. Thus far in our trial, we’ve had two pregnancies after uterus transplant. In both cases, the baby was delivered via cesarean section and mother subsequently underwent hysterectomy — one in 2019 and one in 2020. Both mothers and babies were healthy at discharge.
Advertisement
About the author:Myra Feldman, MD, is Medical Director of Ultrasound at Cleveland Clinic. She has a special interest in female pelvic imaging.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment