Could it unlock the potential for new approaches to treatment?
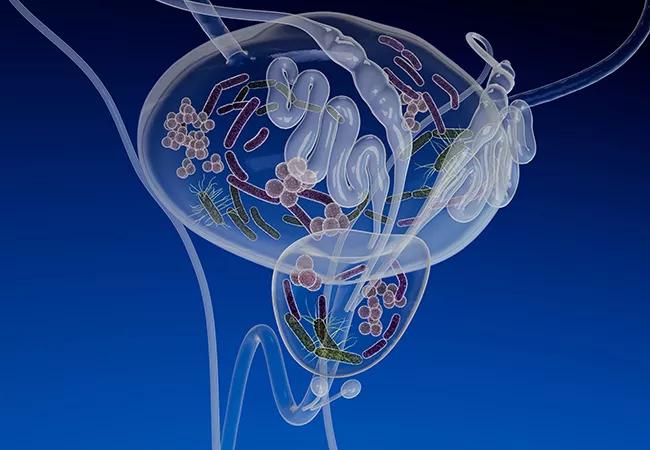
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/88c6eac3-061f-4084-b031-22e01077204b/21-URL-2271032-CQD-650x450-1_jpg)
21-URL-2271032 CQD 650×450
Cleveland Clinic researchers have identified distinct differences in both bacterial and fungal species among women with and without overactive bladder (OAB), suggesting the potential for new approaches to treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
OAB is a common urologic diagnosis, predominantly characterized by the symptoms of urinary urgency and frequency.
The novel microbiome and “mycobiome” findings came from two separate studies conducted by a multidisciplinary Cleveland Clinic team led by urology resident Glenn T. Werneburg, MD, PhD. He’ll be presenting the data at the upcoming American Urological Association meeting on May 1st and April 29th, respectively.
“Having a better understanding of the microbiota involved in OAB opens up the possibility that modulating them can augment our current treatments or perhaps even serve as treatment in and of itself. This is an exciting opportunity for further study,” Dr. Werneburg says.
Previous studies looking at bacterial species in OAB have yielded conflicting results, while virtually no prior OAB work has focused on fungi. “Cleveland Clinic brings together researchers with different areas of expertise that allow them to approach a problem in unique ways,” he notes.
The study investigating bacterial species involved 46 adult women with OAB and 32 healthy controls without urologic diagnoses. All provided clean catch urine specimens, which were subjected to next-generation sequencing and determination of microbial heterogeneity.
Microbiota were detected in all urine samples, but the species differed significantly. Firmicutes were less abundant (P = 0.005) and Proteobacteria were more abundant in the OAB group than the control group (P < 0.05). Escherichia/Shigella taxa were more abundant in the OAB group (P < 0.001), and Lactobacillus taxa were more abundant in the control group (p<0.05).
Advertisement
No Escherichia/Shigella taxa were more abundant in the control group, and no Lactobacillus taxa more abundant in the OAB group.
“There were other differences but not as dramatic as these,” Dr. Werneburg observed.
In a separate analysis of urinary fungi, clean catch urine samples were subjected to next-generation sequencing using internal transcribed spacer (ITS) primers of nuclear DNA to capture fungii, and fungal heterogeneity was determined.
Fungi were detected in all the samples. In the OAB patients the predominant phylum was Ascomycota, whereas Basidiomycota predominated in healthy controls. Malassezia taxa was less abundant (12% OAB, 18% controls, P < 0.05) in the OAB group and Aspergillus was more abundant in the OAB group (14% OAB versus 7% controls, P < 0.05).
“No one has previously looked at fungus in this sort of way. We don’t understand the clinical significance of these fungal patterns in the urine, but the findings present opportunities for future investigation. “This study is the first to show that there’s a clear difference in fungal variability between these two populations,” Dr. Werneburg notes.
The findings have potential implications for OAB treatment. “When we give a botulinum toxin injection in the bladder, is there a type of microbial community associated with a better response to therapy in some people? If so, can we change that community methodically and augment their treatment response? We think that could be a possibility.”
Adding to this, Sandip Vasavada, MD, Urologic Director of the Center for Female Urology and Reconstructive Pelvic Surgery and a co-author on the studies, says, “Many patients with overactive bladder do respond to behavioral modifications or medications, but in cases of refractory overactive bladder, when we consider third-line therapies such as bladder injection of onabotulinumtoxinA and sacral and peripheral neuromodulation, data such as these could potentially predict therapeutic success or failure,” he says.
Advertisement
“We are always looking for better ways to understand patients’ responses to therapies, and this is an area that hasn’t been characterized before in this context,” Dr. Vasavada notes, adding that most research into the microbiome and mycobiome has focused on the gut, and not the bladder.
The next steps include increasing the sample size and collecting data to increase statistical power of the comparisons. In addition, “we want to stratify patients based on their response to treatments, and how the bacteria present in their urine may be associated with their response,” says Dr. Werneburg.
And there’s another intriguing question: Is OAB an infectious disease? That’s a farther-away possibility, but if signs point that way the current Cleveland Clinic team of clinical urologists and microbiologists could bring infectious disease specialists into the work. “We have an interdisciplinary relationship between clinicians and basic scientists and a unique infrastructure with core facilities that allow us to conduct cutting-edge experiments,” Dr. Werneburg says.
Aaron Miller, PhD, assistant staff with Cleveland Clinic’s Lerner Research Institute and Glickman Urologic & Kidney Institute, is senior author on both studies.
Advertisement
Advertisement
Study leverages data from the ROSETTA trial
New care path supports obstetric patients with bladder dysfunction
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.