Discovery of new MS subtype suggests that the axon itself may be primary site of injury
By Daniel Ontaneda, MD, MSc, and Bruce Trapp, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Multiple sclerosis (MS) is well-established as being a highly heterogeneous disease, and now part of this heterogeneity can be better explained by the discovery of a new MS subtype characterized by the absence of demyelination in cerebral white matter.1 This discovery was made using the rapid brain donation program at Cleveland Clinic, which involves in situ MRI followed by pathological examination of the brain within six hours of death.
We and our collaborators found that 12 of 100 cases of MS received for brain donation had no cerebral white matter demyelination but did have loss of myelin in the cerebral cortex and spinal cord, prompting us to name this new subtype myelocortical multiple sclerosis (MCMS) (Figure 1). We then conducted a comparative study between the 12 patients with MCMS and 12 cases of typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration and Expanded Disability Status Scale score.
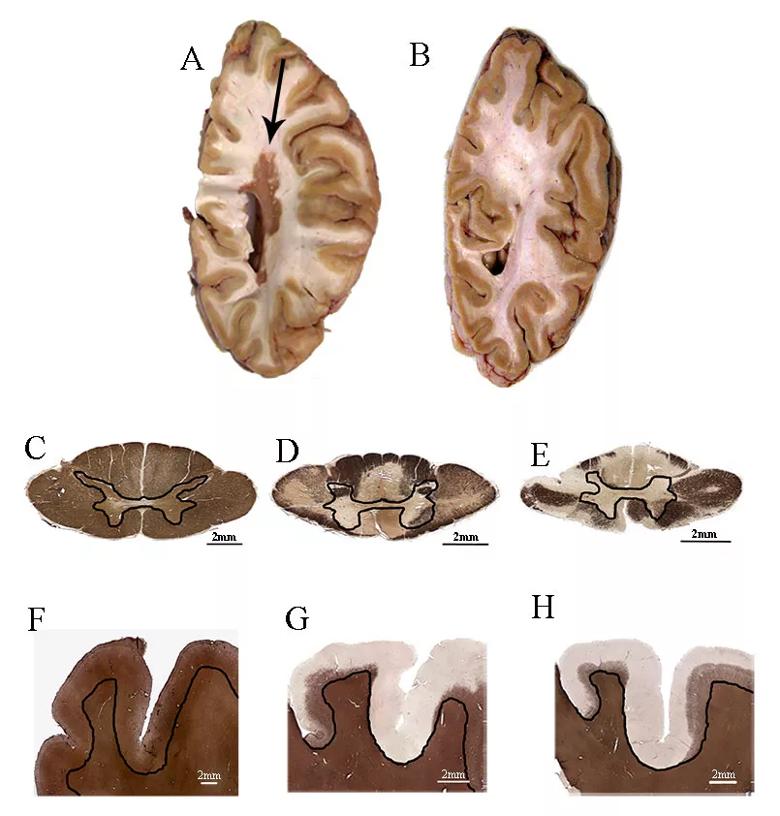
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3fba30e1-dd99-4e9f-a8d4-8237e31ea879/18-NEU-5687-myelocortical-multiple-sclerosis-fig1_jpg)
Figure 1. Demyelination in myelocortical MS and typical MS. (A and B) Centimeter-thick slices from (A) a typical MS brain containing a large white matter lesion (arrow) and (B) a myelocortical MS brain without white matter lesions. (C) A normally myelinated spinal cord section labeled with anti-PLP antibodies. (D and E) Spinal cord demyelination was detected in tissue sections from individuals with typical MS (D) and myelocortical MS (E). (F) Normally myelinated cortex labeled with an anti-PLP antibody. (G and H) Subpial cortical lesions in typical MS (G) and myelocortical MS (H). Black lines separate spinal cord gray and white matter (C-E) and cortical and subcortical white matter (F-H). PLP = myelin proteolipid protein. Reprinted from Trapp et al., Lancet Neurol.1 Copyright 2018, with permission from Elsevier.
Advertisement
Clinical, MRI and histological features were compared between MCMS and typical MS cases. No significant differences were found in relation to the clinical history or MRI features of individuals with MCMS versus typical MS. The amount of cortical demyelination was similar between the groups (4.45 percent in MCMS vs. 9.74 percent in typical MS; P = .5), and spinal cord demyelination was present in both groups, although a greater demyelinated area was found in typical MS as compared with MCMS (13.8 percent vs. 3.8 percent, P = .01). MRIs were also compared between MCMS and typical MS patients, with no significant differences found between the groups.
Despite the absence of demyelination in white matter, cortical neuronal density was decreased in MCMS as compared with control cases without neurological disease. Neuronal densities were examined in layers III, V and VI (cortical projection neurons), specifically from regions not receiving from or projecting to the spinal cord (inferior frontal gyrus, superior temporal gyrus, superior insula, inferior insula and cingulate gyrus) (Figure 2 and Table 1). This analysis provides evidence that neurodegeneration, manifested as cortical neuronal loss, occurs in MCMS independently from cerebral white matter demyelination. This is a significant finding, as it is the first pathological evidence that demyelination and neurodegeneration can occur as independent events in MS.
These results have significant implications on how we view the disease and how we treat MS. They suggest that prevention of white matter lesions alone may not be sufficient to prevent neurological disability. Going forward, the mechanisms of neuronal loss require further exploration for identification of pathways that lead to neurodegeneration. The results also suggest that neuroprotective medications will be needed, in addition to anti-inflammatory medications, to fully treat the disease.
Advertisement
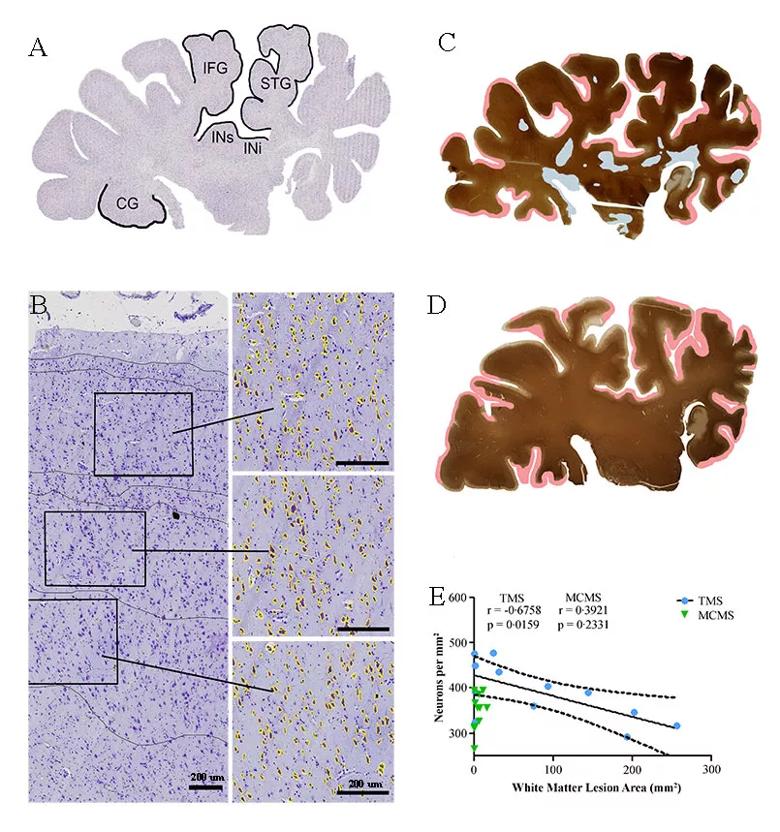
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bec16fb8-6952-484e-972a-3931a95f26d2/18-NEU-5687-myelocortical-multiple-sclerosis-fig2_jpg)
Figure 2. Neuronal loss in the absence of cerebral white matter demyelination. (A) A cresyl violet-stained control hemispheric section from an individual classed as having typical MS. Neuronal densities were compared in cortical layers III, V and VI in each of the five labeled areas (IFG = inferior frontal gyrus; STG = superior temporal gyrus; INi = inferior insula; INs = superior insula; CG = cingulate gyrus). (B) Neurons with an area greater than 60 µm2 (yellow) are shown in a representative image from the superior temporal cortex. (C and D) Labeling for myelin proteolipid protein and the distribution of demyelinated lesions (white matter demyelination is highlighted in blue, subpial demyelination in pink) in hemispheric sections from individuals with typical MS (C) and myelocortical MS (D). (E) A significant correlation between reduced cortical neuronal density and increased cerebral white matter lesion volume was found in typical MS but not in myelocortical MS (dashed lines indicate 95 percent confidence interval). Reprinted from Trapp et al., Lancet Neurol.1 Copyright 2018, with permission from Elsevier.
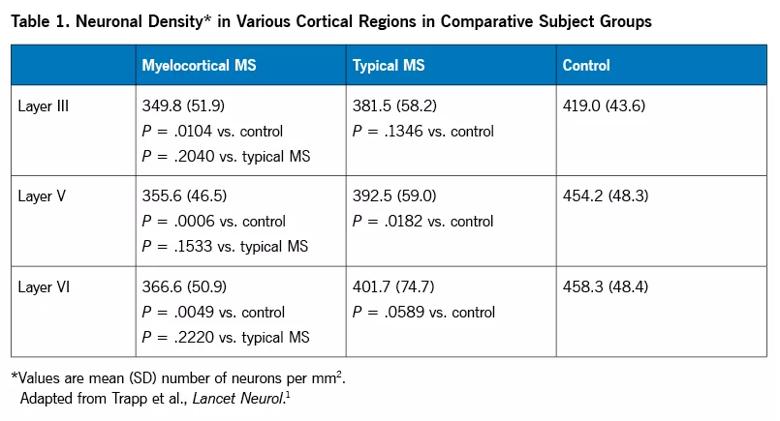
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/990e5c59-485f-4600-9895-62ff00860852/18-NEU-5687-myelocortical-multiple-sclerosis-table1_jpg)
Areas with normal myelin content but with abnormal signal on T2-weighted MRI, T1-weighted MRI and magnetization transfer ratio (MTR) images were identified and then histologically examined and compared with normal-appearing white matter. The most striking finding was the presence of swollen myelinated axons in the T1/T2/MTR abnormal regions. This significant observation suggests that brain white matter MRI abnormalities that are thought to reflect loss of myelin can reflect pathology of myelinated axons. The findings that axonal pathology underlies what otherwise appear to be typical MS lesions may suggest that the axon itself, rather than myelin, may be the primary site of injury in MS. The next step of our research is to further interrogate these axons with electron microscopy and examine the underpinnings of why axonal swelling occurs.
Advertisement
Perhaps one of the most striking conclusions of our study is the relatively poor specificity of MRI for myelin content in cerebral white matter. The finding that almost 12 percent of patients with MS could have intact cerebral white matter will have important implications for the field.
A significant focus is now being placed on trials examining remyelinating agents, and many of those trials examine changes in purported myelin-sensitive imaging in white matter brain lesions. MCMS patients will not be informative for such studies targeting myelin content in white matter.
The findings in MCMS patients may also be leveraged to look for MRI markers that are more specific to myelin using fixed tissue, with the aim of then translating these markers for use in live patients.
The ultimate goal of this research will be identification of MCMS patients in life, which may help discriminate differential treatment effects and perhaps better inform prognosis.
MCMS is a novel subtype of MS with intact brain white matter myelin and presence of cortical and spinal cord demyelination. Clinical and MRI features do not differentiate MCMS and typical MS, but these findings have significant implications for how we view the disease. We plan to leverage these results to identify better myelin markers, understand the role of the axon in MS, identify MCMS in live patients and further develop neuroprotective therapies in MS.
Advertisement
Dr. Ontaneda is a neurologist with Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. Dr. Trapp is Chair of the Department of Neurosciences in Cleveland Clinic Lerner Research Institute.
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology