Phase 3 ODYSSEY-HCM trial of mavacamten leaves lingering questions about potential broader use
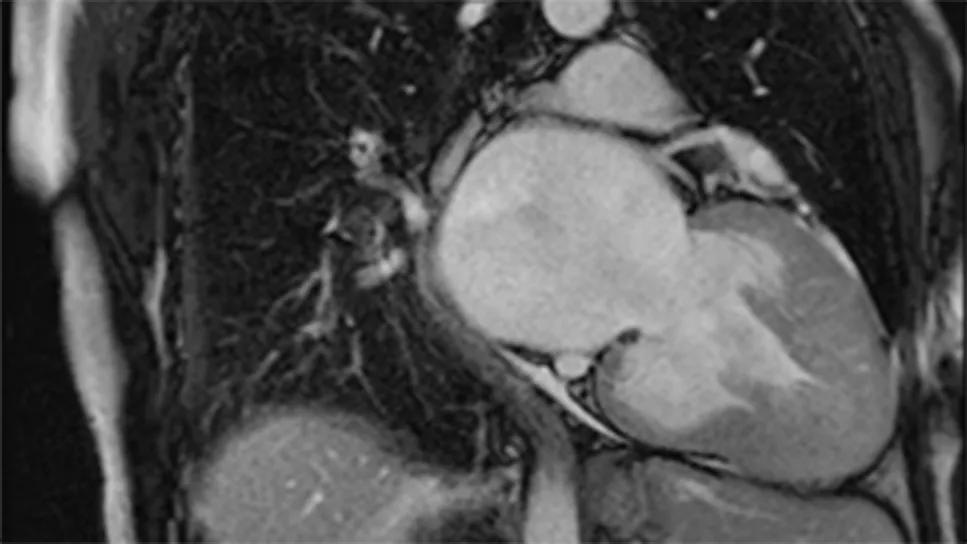
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f1d9bbd0-03ac-4cec-b812-cccee9c7336e/nonobstructive-hypertrophic-cardiomyopathy)
imaging study of a heart with nonobstructive hypertrophic cardiomyopathy
No significant improvements in functional capacity or patient-reported health status were observed after 48 weeks of mavacamten therapy among patients with symptomatic nonobstructive hypertrophic cardiomyopathy (HCM) in ODYSSEY-HCM, the first phase 3 investigation of a cardiac myosin inhibitor for nonobstructive HCM. Secondary analyses of the trial, however, showed that mavacamten was associated with significant improvements in cardiac biomarkers and with favorable cardiac remodeling on echocardiography.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So reported Milind Desai, MD, MBA, and coinvestigators with the ODYSSEY-HCM trial in late-breaking science sessions at the European Society of Cardiology (ESC) Congress 2025. The primary ODYSSEY-HCM results were simultaneously published in the New England Journal of Medicine, with results of the biomarker and echocardiography analyses published in the Journal of the American College of Cardiology.
“In nonobstructive HCM, where left ventricular outflow tract (LVOT) obstruction is not present, the effect of cardiac myosin inhibitors on hemodynamics and ventricular efficiency may be limited, which could explain the lack of clinically meaningful improvements observed in ODYSSEY-HCM,” says Dr. Desai, Medical Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center, who presented the primary and secondary analyses at the ESC Congress. “At the same time, the positive findings from the biomarker and echocardiography secondary analyses suggest mechanistic insights into potential utility for mavacamten in nonobstructive HCM.”
The ODYSSEY-HCM trial was undertaken following regulatory approval of mavacamten for treating symptomatic obstructive HCM. Although LVOT obstruction is the chief cause of symptoms in the 50% to 70% of patients with HCM in whom it is present, the sizable share of HCM patients without obstruction can also develop symptoms, which may be related to diastolic dysfunction, left ventricular (LV) hypercontractility, microvascular ischemia and other nonobstructive causes. No therapies have shown consistent efficacy for easing symptoms, improving quality of life or expanding functional capacity for patients with nonobstructive HCM.
Advertisement
Because mavacamten, as a cardiac myosin inhibitor, targets the sarcomeric defect implicated in HCM, interest has arisen in using this agent to alleviate hypercontractility in HCM and thereby boost LV efficiency. This would broaden the drug’s benefits beyond easing LVOT obstruction, perhaps offering meaningful clinical utility in symptomatic nonobstructive HCM.
Indeed, the phase 2 MAVERICK-HCM study of mavacamten in symptomatic adults with nonobstructive HCM found significant improvements in cardiac biomarkers — NT-proBNP and cardiac troponin I — and post hoc analysis revealed a subgroup of patients who showed favorable changes from baseline in peak oxygen consumption (pVO2) and quality of life (as measured by the Kansas City Cardiomyopathy Questionnaire-23 Clinical Summary Score [KCCQ-23 CSS]) with mavacamten relative to placebo.
MAVERICK-HCM prompted the phase 3 ODYSSEY-HCM investigation (NCT05582395), which enrolled 580 adults with symptomatic nonobstructive HCM from 22 countries.
Stringent entry criteria ensured that patients had nonobstructive HCM confirmed by rigorous core laboratory echocardiographic assessments (performed by the Cleveland Clinic Coordinating Center for Clinical Research [C5Research]). Eligible patients had NYHA class II or III symptoms as well as preserved (≥ 60%) LV ejection fraction (LVEF) and no significant LVOT obstruction at rest or with provocation.
Participants were randomized 1:1 in double-blind fashion to placebo or mavacamten starting at 5 mg/day, which was titrated up to 15 mg/day based on LVEF. Sham titration was used for placebo recipients.
Advertisement
The patient population was 46% female and had a mean age of 56 years and mean HCM disease duration of roughly 10 years. At baseline, patients had elevated NT-proBNP and cardiac troponin I, diastolic dysfunction and reduced exercise capacity (mean pVO2 of 18.2 mL/kg/min), collectively indicating substantial disease burden.
The study had dual primary endpoints: change in pVO2 and change in patient-reported health status (assessed by KCCQ-23 CSS) from baseline to week 48.
At 48 weeks, mavacamten demonstrated no statistically significant improvement over placebo in increases in pVO2 (difference of 0.47 mL/kg/min; P = .066) or KCCQ-23 CSS (difference of 2.7 points; P = .056). Secondary endpoints also failed to demonstrate significant benefits warranting further statistical testing. Both groups showed some symptom improvement, which may have reflected enhanced background care during the study.
Mavacamten was associated with more frequent treatment interruptions (25.7% vs. 7.6%) and permanent discontinuations (10.7% vs. 5.8%) compared with placebo. Reductions in LVEF below 50% occurred in 21.5% of mavacamten recipients versus 1.7% of placebo recipients, with 2.4% (all in the mavacamten arm) experiencing LVEF of 30% or below, requiring drug discontinuation. In most patients, LVEF recovered after drug interruption. Serious adverse events were more common in the mavacamten arm than the placebo arm, with congestive heart failure occurring in 6.6% versus 1.7%, respectively, and atrial tachyarrhythmias in 4.2% versus 3.4%, respectively.
Advertisement
Despite the lack of improvements in its dual primary endpoints, ODYSSEY-HCM enabled assessment of additional clinically relevant measures, including cardiac biomarkers.
The cardiac biomarker secondary analysis, prompted in part by biomarker findings from MAVERICK-HCM, focused on changes in NT-proBNP and high-sensitivity cardiac troponin I over the 48 weeks of treatment.
Levels of these biomarkers were elevated at baseline, with a median NT-proBNP of 917.5 ng/L and a median troponin I of 29.1 ng/L, indicating significant myocardial stress and injury in this population.
After 48 weeks, mavacamten treatment led to a 58% reduction in NT-proBNP (P < .001) and a 51% reduction in troponin I (P < .001). These changes occurred early, by week 23, and were sustained through week 48. In contrast, the placebo group showed no significant biomarker changes.
Stratification by quartiles of biomarker change showed that patients with the largest NT-proBNP reductions also had the greatest improvements in pVO2, diastolic function (E/eʹ ratio), left atrial volume index and maximal LV wall thickness. Similar trends were seen with troponin I reductions, including associations with septal E/eʹ and reductions in wall thickness and LVEF, although changes in patient-reported outcomes and NYHA class were less consistent.
Patients with more modest biomarker reductions were more likely to experience atrial arrhythmias and LVEF reductions below 50%. Notably, mavacamten recipients with LVEF < 50% had significantly smaller reductions in NT-proBNP and troponin I, underscoring the importance of careful dose titration and monitoring.
Advertisement
The other secondary analysis assessed blinded echocardiographic changes in noninvasive hemodynamics and in left atrial and left and right ventricular function.
Patients’ baseline imaging revealed significant disease burden, with an average maximal LV wall thickness of 20.8 mm, LV mass index of 122.3 and impaired diastolic function (average E/eʹ of 13.3). LV global longitudinal strain was reduced (–13.2%), and left atrial volume index was elevated (43.5 mL/m²), indicating advanced cardiac remodeling.
Left ventricular changes. After 48 weeks, mavacamten therapy resulted in significant reductions in maximal LV wall thickness (–2.1 mm), LV mass index (–5.7 g/m²) and average E/eʹ (–1.6) relative to baseline (P < .05 for all), compared with no significant change with placebo. Although there was a modest decrease in LVEF with mavacamten (–5.3%; P < .01), mean LVEF remained within normal limits. Notably, in the 73.3% of mavacamten recipients who maintained LVEF ≥ 50% throughout the study, LV global longitudinal strain improved modestly (–0.6%; P < .05), indicating enhanced systolic function despite the LVEF reduction.
Left atrial and right ventricular function. Mavacamten also improved left atrial functional measures, including reservoir strain (+0.6%) and conduit strain (–1.2%) (P < .05 for both), with a significant reduction in left atrial volume index among patients without atrial fibrillation (–4.4 mL/m²; P = .001). Right ventricular parameters remained within normal ranges, although some were statistically lower in the mavacamten arm than in the placebo arm.
Echocardiographic improvements were observed regardless of atrial fibrillation status or episodes of LVEF reduction. Echocardiographic changes consistent with favorable cardiac remodeling were significantly correlated with NT-proBNP levels but only weakly correlated with KCCQ-23 CSS scores and pVO2.
“Forty-eight weeks of mavacamten therapy did not significantly impact exercise capacity or patient-reported health status in these symptomatic individuals with nonobstructive HCM and advanced disease burden,” observes Dr. Desai. “These results underscore the distinct pathophysiology of nonobstructive versus obstructive HCM. However, the secondary analyses revealed marked improvements in cardiac biomarkers and favorable cardiac remodeling in mavacamten recipients, with these beneficial effects coinciding in many patients. These effects are consistent with findings in studies in obstructive HCM.”
He and his co-authors note that the secondary analyses’ results raise the possibility that more sensitive endpoints may be needed to assess clinical benefit in studies of nonobstructive HCM. They identify several questions that remain, including:
The researchers call for larger studies with longer follow-up to address these questions. They note that ongoing trials with other myosin inhibitors and novel therapies are exploring additional treatment avenues for nonobstructive HCM.
“Although the lack of efficacy of mavacamten in nonobstructive HCM is disappointing, we are always proud of well-conducted trials regardless of the outcome, and negative results often lead to medical progress,” notes ODYSSEY-HCM senior author Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular and Thoracic Institute. “The pathophysiology of nonobstructive HCM is clearly different from obstructive HCM and will require other approaches. Dr. Desai and the rest of the team can now focus on understanding everything that can be learned from the ODYSSEY-HCM trial, and the changes in biomarkers and echocardiography findings are an important first step.”
ODYSSEY-HCM was funded by Bristol Myers Squibb, which markets mavacamten. Dr. Desai reports research and consulting agreements with Bristol Myers Squibb. Dr. Nissen reports consulting for and conducting clinical trials funded by Bristol Myers Squibb and other pharmaceutical companies but that he receives no personal compensation for these activities.
Advertisement
End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential
Cardiac imaging substudy is the latest paper originating from the VANISH trial
Vigilance for symptom emergence matters, a large 20-year analysis reveals
5% of flagged ECGs in real-world study were from patients with previously undiagnosed HCM
High composite score in myectomy specimens signals worse prognosis
Few patients report left ventricular dysfunction or heart failure after one year
Avoidance of septal reduction therapy continues while LVEF dysfunction remains infrequent
New risk score pools factors that may predict adverse outcomes in the uncommon phenotype