Pattern and intensity of autofluorescence differs between normal and hyperfunctioning parathyroid glands
Hyperfunctioning and normofunctioning parathyroid glands exhibit different patterns and intensity of autofluorescence when using near-infrared fluorescence imaging (NIFI), a recent study finds. This modality could be used in the context of thyroidectomy and parathyroidectmoy to predict parathyroid function, aiding in surgical decision making.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Even for the most experienced surgeons, intraoperative exploration of parathyroid glands can be challenging,” states Eren Berber, MD, a surgeon with Cleveland Clinic’s Department of Endocrine Surgery. “Most commonly, neck ultrasound and sestamibi scans are used to find localized disease. But even these have limited accuracy.”
Other imaging modalities have been proposed, including the use of amniolevulinic acid or a handled gamma probe. Until now, new modalities have failed to predict parathyroid function and had unwanted side effects, including injection-related complications, radiation exposure and photosensitivity.
Previous research established the feasibility of testing the autofluorescence from parathyroid glands intraoperatively, but this is the first study to investigate the technology for use in differentiating between glands that function normally from those with hyperfunctionality.
“Interestingly, our results contradict a 2016 study, which measured higher autofluorescence intensity in hypercellular glands compared to normal glands,” notes Dr. Berber.
To explore the utility of NIFI in the operating room, we added it to our standard of care in 50 parathyroid cases. We measured the autofluorescence intensities, and selected a representative photo in the field for further analysis.
Intraoperatively, 192 parathyroid glands were identified via autofluorescence. Twenty-six percent of these parathyroid glands were identified by NIFI prior to dissection and visual identification, which may have reduced operating time.
Advertisement
Hyperfunctioning parathyroid glands had lower mean autofluorescence intensity, and more often exhibited a heterogeneous pattern of autofluorescence compared to normofunctioning parathyroid glands. Upon further evaluation, the glands with low-intensity, heterogeneous autofluorescence, including increased cellularity, patchy areas of fibrosis, oxyphilic cell clusters and areas of hematoma.
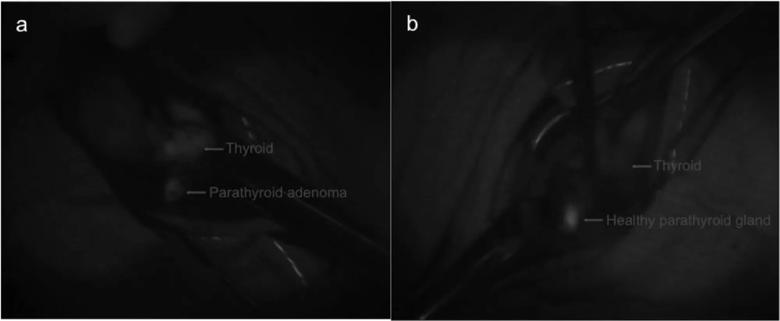
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/35bfbba3-47d4-4a6d-9dc3-3ff08dad8970/Figure-1a_jpg)
Intraoperative photos showing a heterogeneous, lower intensity autofluorescence detected from an excised parathyroid adenoma (A) versus a preserved, suppressed parathyroid gland (B). The normalized autofluorescence intensities of these glands were 2.0 and 5.1, respectively. The patient’s parathyroid hormone levels normalized postoperatively.
“Although we still do not understand the exact nature of parathyroid fluorescence, pathologic parathyroid glands may lose the ability to emit strong, homogeneous autofluorescence,” Dr. Berber hypothesizes.”
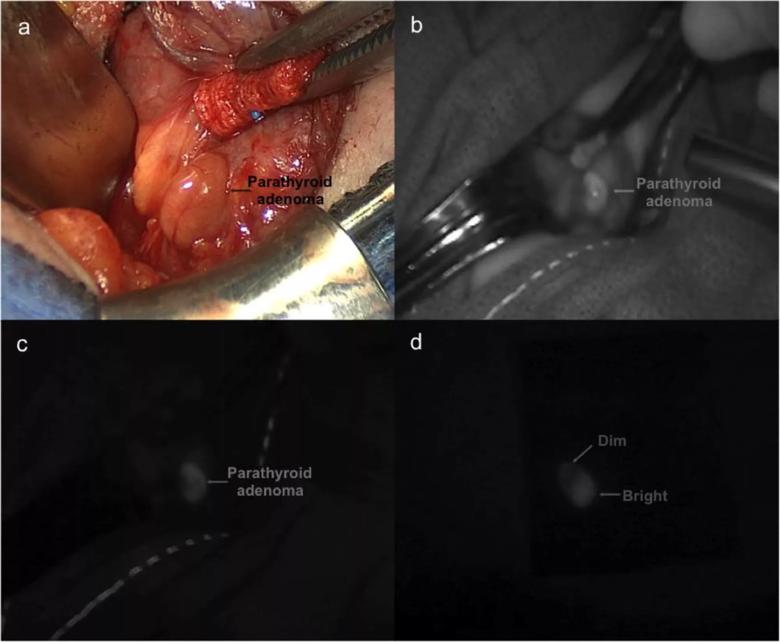
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/55431e1d-7357-42b0-b5ae-5721aa44a777/Figure-2_jpg)
Intraoperative captures of a parathyroid adenoma. On exploration (A), the gland was larger and firmer than normal. After turning down the operating room lights, the gland was identified using the white-light mode (B) of the near-infrared fluorescence system followed by autofluorescence imaging (C). The heterogeneous autofluores- cence detected from this gland was noted to persist ex vivo after excision (D).
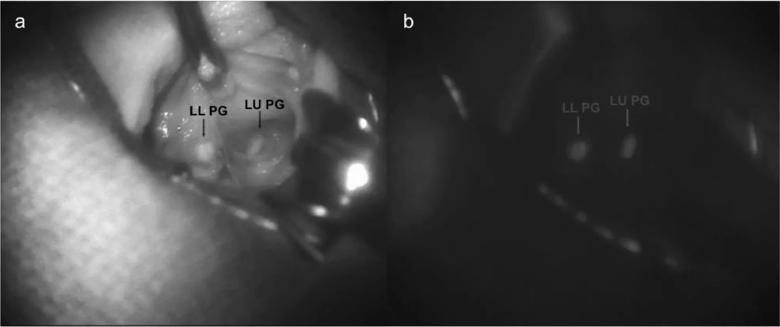
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/092af625-4130-439c-9202-f9ed21a8f23d/Figure-3_jpg)
Intraoperative photos of 2 suppressed parathyroid glands. After localization in white-light mode (A), autofluorescence imaging (B) was performed. Bright and homogeneous autofluorescence was detected from both glands. LL, left lower; LU, left upper; PG, parathyroid gland.
Advertisement
Primary hyperparathyroidism can be caused by adenoma, hyperplasia, and rarely, by parathyroid cancer. The syndrome is most common in post-menopausal women. In fact, parathyroidectomy rates are twice as high among woman compared to white men. The estimated prevalence of hyperparathyroidism is three per 1,000 in the general population, and parathyroidectomy rates in are twice as high among white women compared to white men.
Asymptomatic patients, with only mildly elevated serum calcium levels, may be treated conservatively. Surgical removal of diseased parathyroid glands is the only definitive treatment. If left untreated, serious complications can include nephrolithiasis, chronic kidney disease and osteoporosis. Intraoperative autofluorescence imaging of parathyroid glands is one of the most significant breakthroughs in parathyroid surgery, with a number of hospitals involved in pioneering work about this technology. Cleveland Clinic has one of the first hospitals to be involved in this technology and has been assessing the utility of this modality prospectively since 2016.
Dr. Berber’s areas of interest include laparoscopic and robotic liver surgery, laparoscopic liver tumor ablation, robotic surgery, conventional and minimally invasive endocrine surgery (thyroid, parathyroid, adrenal and pancreas), robotic thyroidectomy, robotic adrenalectomy and surgical ultrasound. He is a active member of numerous surgical societies, including American College of Surgeons and serves in multiple committees, and was on the program committee for the first symposium on parathyroid fluorescence in Geneva, Switzerland, in March 2019.
Advertisement
Note: Images repurposed with permission from Elsiver, originally published in: Kose E, Kahramangil B, Aydin H, Donmez M, Berber E. Heterogeneous and low-intensity parathyroid autofluorescence: Patterns suggesting hyperfunction at parathyroid exploration. Surgery. 2019 Feb;165(2):431-437.
Advertisement
Advertisement
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D
Patients spent less time in the hospital and no tumors were missed
A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications