Raising awareness of a common manifestation
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Neurologic involvement is well documented in ANCA-associated vasculitis (AAV), but its prevalence has not been well characterized. My colleagues from the Vasculitis Clinical Research Consortium (VCRC) and I recently presented data at the 2021 American College of Rheumatology Convergence from a multicenter longitudinal observational study that allows us to understand more clearly the prevalence and types of neurological involvement and its associations with other manifestations of vasculitis.
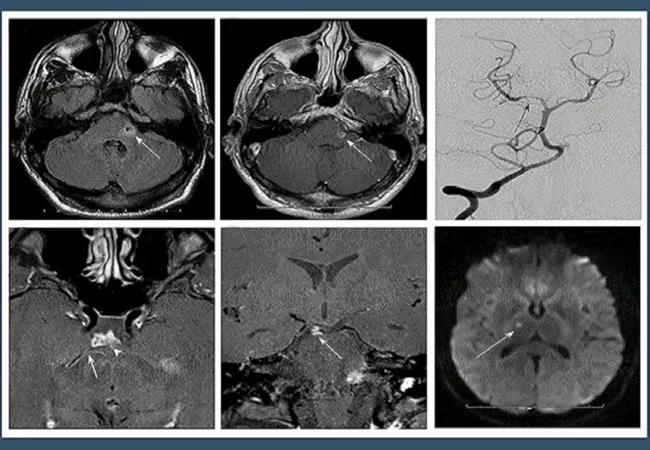
Our study analyzed data from 1368 adult patients with AAV (granulomatosis with polyangiitis [GPA], microscopic polyangiitis [MPA] or eosinophilic granulomatosis with polyangiitis [EGPA]) collected from 2006-2021. Just over a third of patients had neurological involvement. Of this 34%, 46.2% had EGPA, 46% had GPA and 7.8% had MPA. In the overall cohort, 27.3% of patients experienced peripheral nervous system (PNS) involvement and 3.4% had neurological involvement in the central nervous system (CNS) (3.2% unclassified). Most patients with CNS involvement had GPA (78% compared with 19% in EGPA and 2% in MPA), while EGPA was the most common diagnosis for patients with PNS involvement (51% compared with 40% in GPA and 8.8% in MPA).
We observed no significant difference in rates of neurological involvement by patient sex or race, though the cohort was overwhelmingly white (88.7%). The mean age at diagnosis was higher for patients with neurological involvement than without (51.4 vs. 47.0 years, P < 0.001).
Advertisement
We also discovered that neurological involvement was significantly associated with skin (49.4% vs. 29.5%, P <0.001) and cardiovascular (15.5% vs. 7.2%, P < 0.001) involvement as well as venous thrombosis (12.8% vs. 8.6%, P = 0.016). Neurological involvement was negatively associated with renal (45.6% vs. 55.9%, P < 0.0001) and eye (20% vs. 28%, P < 0.001) involvement.
In patients with GPA, neurological involvement was associated with musculoskeletal, skin and kidney involvement and venous thromboses. Patients with EGPA were more likely to experience skin and kidney issues if they had neurological involvement. Patients with MPA with neurological involvement were more likely to have constitutional and musculoskeletal symptoms.
Finally, we found that patients who experienced neurological involvement were more likely to have P-ANCA pattern (43.1% vs. 31.2%, P = 0.008) and anti-MPO (44.4% vs. 30%, P < 0.001) compared with patients without neurological involvement.
These data demonstrate that clinicians should consider neurological involvement common in their patients with AAV, especially in those with EGPA. Neurological symptoms like symmetrical polyneuropathy, paresis, headaches and cognitive impairment should be considered potential evidence of vasculitis in patients with other classic signs of the disease as well as complications to watch for in patients with established diagnoses. The relationships between neurological involvement and other manifestations of disease observed in this study warrant further investigation.
Advertisement
Collaboration with colleagues in neurology is critical for the rheumatologist treating patients with AAV. Cleveland Clinic’s Center for Vasculitis Care and Research collaborates with the Cerebrovascular Center in the Neurological Institute to determine the most appropriate course of treatment for these patients.
Dr. Hajj-Ali is Associate Director of the Center for Vasculitis Care and Research at Cleveland Clinic.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis