An overview of case reports and management
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Nonthrombotic pulmonary embolism (NTPE) is uncommon and can be difficult to diagnose. My colleagues and I recently reviewed this complete or partial occlusion of the pulmonary vasculature resulting from inorganic particulate matter and foreign bodies in Chest. The below images demonstrate accidental embolization from catheter tips and guidewires.
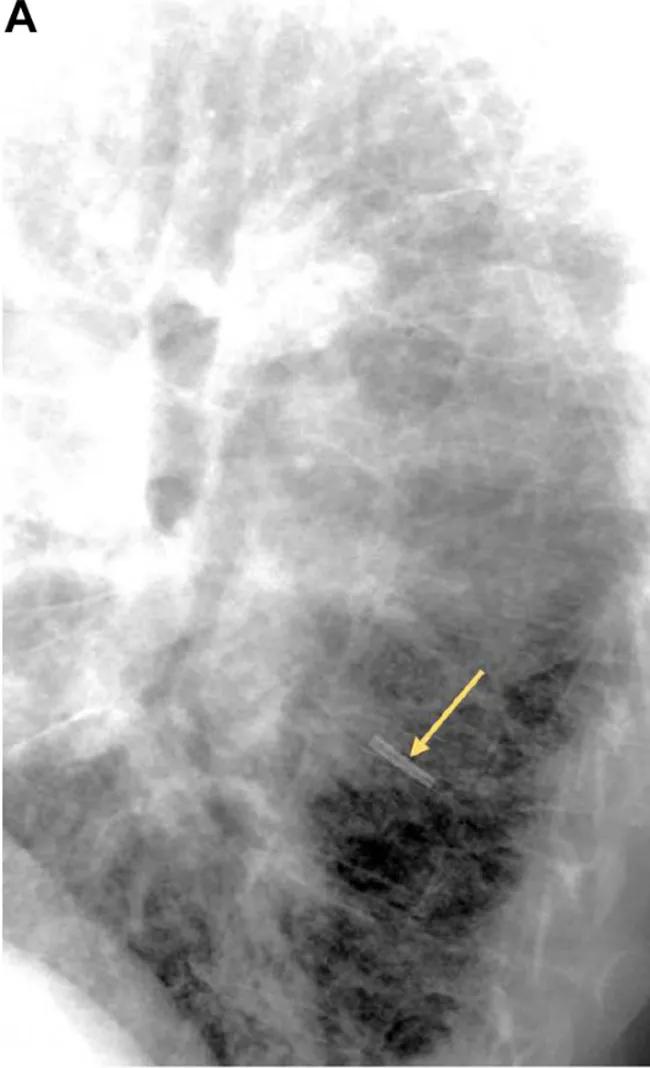
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b422e4a7-0996-4f4e-bd67-e70ba2c4e8d2/18-PUL-4584-Mehta-NPTE-Inset-Image-01-650pxl-width_jpg)
This lateral chest radiograph shows an embolized central venous catheter (CVC) tip in the left lower lobe sub- pulmonary artery branch. Intensivists commonly use CVCs for venous access. Potential complications include phlebitis, central line-associated bloodstream infections and catheter fracture with or without downstream embolization. Tip fracture and embolization like the example above can occur with any type of catheter, sometimes due to “pinch-off” syndrome, when a catheter placed in the subclavian vein gets wedged between the clavicle and the rib, leading to compression, transection and embolization.
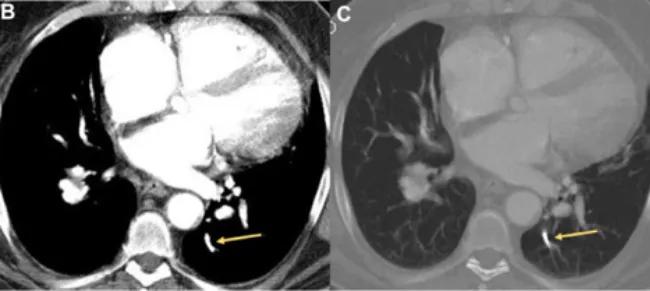
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b7c9017b-59d5-4250-9e5c-2403af10b7d9/18-PUL-4584-Mehta-NPTE-Inset-Image-02-650pxl-width_jpg)
These contrast-enhanced axial CT images (B, soft tissue window; C, bone window) at the level of the ventricles show an embolized catheter tip in the left lower lobe posterior sub-segmental artery.
NTPE has also been reported to occur when removing the guidewire or during catheter exchange. Catheter fragments have been known to lodge in the pulmonary artery, hepatic or brachiocephalic veins, superior vena cava, right atrium and right ventricle.
The below image demonstrates the gold standard of management for this type of NTPE: percutaneous retrieval via the femoral route. This isn’t always possible, and thoracotomy is an option. The image below shows (A) a contrast-enhanced chest CT with a linear radiopaque guidewire in the distal right main pulmonary artery extending into the proximal right lower lobe artery and right interlobar. The angiogram on the right (B) shows cannulation of the right pulmonary artery and fluoroscopic guided retrieval of the guidewire using a snare.
Advertisement
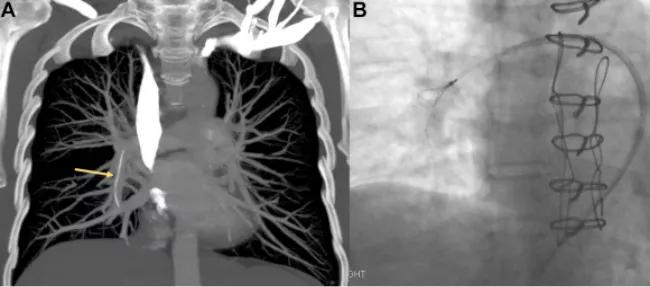
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/73f1b698-ecda-43c5-bfa9-446381bc85f5/18-PUL-4584-Mehta-NPTE-Inset-Image-03-650pxl-width_jpg)
This is a rare occurrence, and patients may present with a wide spectrum of signs and symptoms from none to severe. Accurate diagnosis requires extensive knowledge of imaging modalities and postprocessing tools. Future posts will review other macroscopic emboli like radiation seeds and cement, microscopic emboli like ethiodized oil and silicone embolus and talc granulomatosis.
Cleveland Clinic coauthors include Sanjay Mukhopadhyay, MD, staff, Department of Anatomic Pathology, Derick Asah, DO, resident, and Subha Ghosh, MD, staff, Department of Diagnostic Radiology.
Dr. Mehta is staff in the Department of Pulmonary Medicine.
Images and text republished with permissions from Elsevier. Originally published in Chest.
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Collaborative patient care, advanced imaging techniques support safer immunotherapy management