Ultrasound-guided percutaneous ultrasonic tendon debridement
By Dominic King, DO, and Jason Genin, DO
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Calcific tendinopathy of the shoulder can be a painful and debilitating condition. While several nonoperative treatments have been employed to alleviate this condition (physical therapy, corticosteroid injections, percutaneous lavage, two-needle barbotage procedure and extracorporeal shock wave), arthroscopic surgical debridement is ultimately chosen for many patients with this painful condition.1
We suggest the office-based ultrasound-guided percutaneous ultrasonic tendon debridement procedure as a novel, less invasive alternative to address calcific tendinopathies of the shoulder. This procedure uses a thin metal needle probe that vibrates at 20,000 rpm along with saline irrigation to gently dissolve and aspirate the calcific deposit, while leaving the native normal tendon unaffected.
We have performed more than 400 ultrasound-guided percutaneous tendon debridement procedures. More than 40 were specifically used to treat calcific tendinopathy of the shoulder.
While this procedure has been performed across the country for six years, no studies have been published outlining its use for treatment of calcific tendinopathy of the shoulder.
Here we present a case series of three patients with calcific deposits of the shoulder (see Figures). The patients had calcific deposits of the:
All patients had symptoms of shoulder pain and a reduced range of motion for at least three months. All failed to receive relief from physical therapy or an ultrasound-guided percutaneous lavage procedure with corticosteroid injection.
Advertisement
Each patient underwent an ultrasound-guided percutaneous ultrasonic tendon debridement procedure. At four weeks postprocedure, they all demonstrated improvement in pain and function and did not progress or require further treatment.
All of these patients are at least six months out from the procedure with sustained results. Similar results have been achieved in all patients who have been treated with the same protocol by the authors.
Case 1
A 45-year-old woman with a large calcium deposit of the supraspinatus tendon that caused significant impingement and resulted in superior glenohumeral widening and inferior glenohumeral degenerative changes. Four weeks after treatment with ultrasound-guided percutaneous ultrasonic tendon debridement, she had complete resolution of symptoms, near complete resolution of calcium deposition on plain imaging and did not progress to any further interventional treatment.
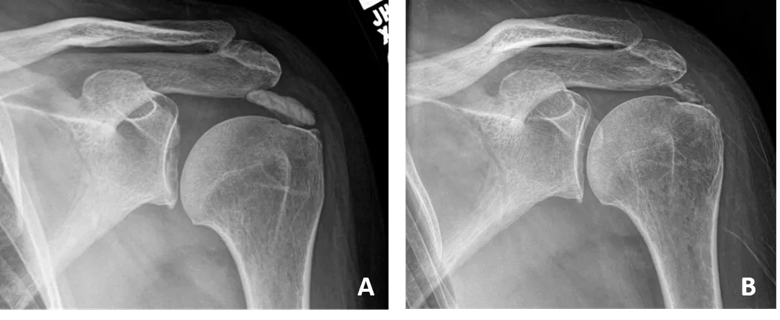
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/61529fe8-b92f-4198-9680-c535a13394b5/Case-1_png)
Image A: Before, Image B: After
Case 2
This 57-year-old woman had a calcium deposit of the pectoralis major tendon that caused pain with reaching and pushing in almost all directions. Four weeks after treatment with ultrasound-guided percutaneous ultrasonic tendon debridement, she had complete resolution of symptoms, complete resolution of calcium deposition on plain imaging and did not progress to further interventional treatment.
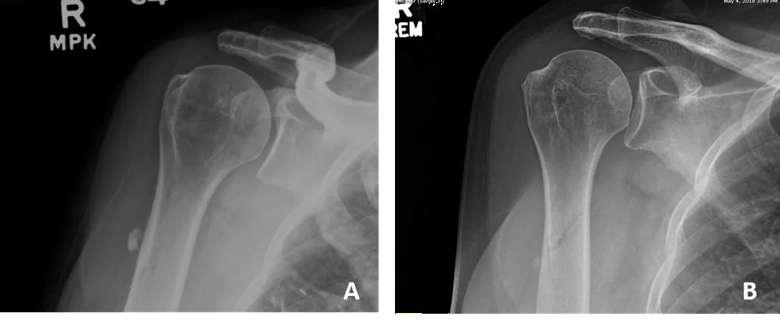
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5ad3a7b4-7d19-4097-957d-75be9dd3d62a/Case-2_png)
Image A: Before, Image B: After
Case 3
A 52-year-old man had a calcium deposit of the subscapularis tendon that caused pain while overhead serving in tennis and with general overhead activity. Four weeks after treatment with ultrasound-guided percutaneous ultrasonic tendon debridement, he had significant reduction of pain and resolution of calcium on plain imaging. By three months, he was able to return to playing tennis, without pain.
Advertisement
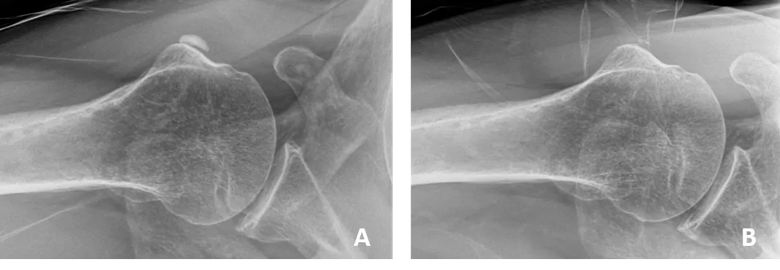
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ec66fd87-a62c-4406-ad7e-49f204c4718a/Case-3_png)
Image A: Before, Image B: After
Based on our 40+ cases using ultrasound-guided percutaneous ultrasonic tendon debridement for the treatment of calcific tendinopathy of the shoulder, we are very optimistic about this option for treating patients experiencing this debilitating condition.
We also find it extremely helpful in the treatment of chronic degenerative tendinosis of the shoulder, elbow, hip, knee, foot and ankle.
Working with the OrthoMidas Episode of Care (OME) team here, we are developing a specific OME tendinopathy module that will help produce a prospective cohort that will allow us to longitudinally track outcomes of these procedures. We welcome your candid discussion regarding this novel therapy and look forward to presenting future outcomes of a larger sample of patients.
Reference
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment