A closer look at the dental challenges
By Michael Horan, MD, DDS, PhD, and Betty Haberkamp, DDS
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Katie Stubblefield, a young woman who received a total face transplant at Cleveland Clinic in May 2017, became the world’s youngest face transplant recipient at age 21. The procedure took 31 hours and required detailed planning and cooperation by a large team of Cleveland Clinic experts. Her team of specialists included surgeons, dentists, anesthesiologists, endocrinologists, ophthalmologists, psychiatrists, infectious disease specialists, physical, occupational and speech therapists, and nurses.
Katie experienced substantial dental challenges during the perioperative period. Here we explain how our dentistry and oral surgery teams worked together to ensure a good long-term outcome for our first total face transplant recipient.
Katie’s trauma was the result of a self-inflicted gunshot wound that left her with just 13 posterior teeth, mostly molars. She initially presented with severely limited mouth opening and oral pain due to her injury and multiple previous reconstructive surgeries. This, along with her inability to see, resulted in a limited ability to perform basic oral hygiene. Limited access also complicated our team’s ability to perform basic restorative care and oral surgical procedures. In addition, due to the nature of her injury, she was unable to completely close her lips (lip incompetence), leading to an inability to control her saliva, which resulted in chronic drooling and contributed to her dry mouth.
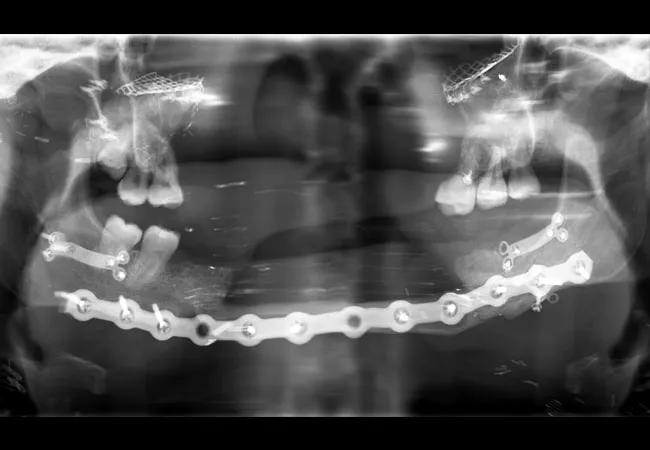
Shortly after arriving at the Cleveland Clinic, Katie began to localize pain to several teeth. Given her condition, obtaining intraoral radiographs proved difficult; to make matters worse, the images were compromised by shadowing of hardware (Figure 1; see large image above). Early on, a decision was made to maintain as many teeth as possible to allow for retention of any future maxillofacial prosthesis. Her maxillary teeth were treated if they were symptomatic, with the understanding that they would be replaced with the transplant. Restoration of teeth was attempted before any extractions were considered. Oral Surgery performed extractions of any infected or non-restorable teeth in the time leading up to the facial transplant (Figure 2). When her transplant was eventually performed, Katie received both the donor’s maxilla and mandible. At the time of the surgery, all of her remaining teeth were removed and she was essentially provided with an entirely new dentition (Figure 3).
Advertisement
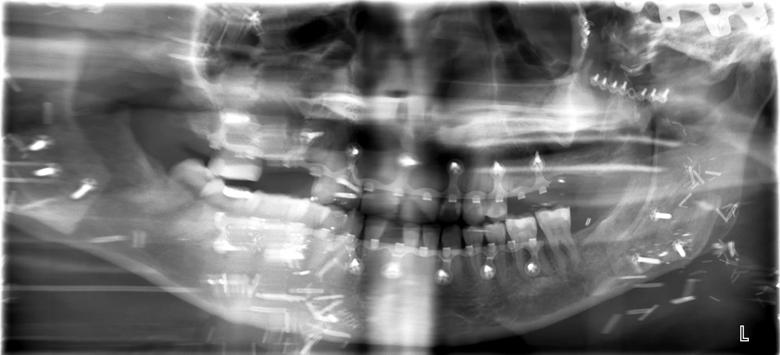
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8abf89d9-b4b7-4511-847f-3af795e9eb2c/Figure-2-Horan_jpg)
Figure 2

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6b1d9168-7b14-4264-af65-6e1d15056631/Figure-3-Horan_jpg)
Figure 3
In the weeks following her transplant, Katie’s dental care was limited in nature due to the need for continuous maxillomandibular fixation. She developed a slight malocclusion and continued to suffer from dry mouth. She was lip competent, but her lack of salivary flow made her prone to dental decay. Fluoride therapy was prescribed to aid in re-mineralization of her new dentition, but decay was still a problem.
From a dental standpoint she is doing well. Her dental restorations have been completed and she continues to receive routine periodic dental exams and hygiene care. As she heals and moves on with her life, it will be necessary to continue to monitor Katie’s facial and oral pain to determine if it is odontogenic so that she can maintain her dentition.
*Katie Stubblefield’s story was featured in detail in the September 2018 edition of National Geographic. The teen attempted suicide with a rifle, which removed her nose, mouth, jaws, part of her forehead, her face and much of her eyesight. Katie and her family chose to share her story in an effort to help others.
Dr. Horan is Section Head of Oral and Maxillofacial Surgery in the Department of Dentistry. Dr. Haberkamp is with the Department of Dentistry and serves as Program Director of the Dental General Practice Residency program.
Advertisement
Advertisement

Analysis of HNSCC patients shows HPV status to be predictive of higher abundance of oncobacteria within the tumor

Case study illustrates the potential of a dual-subspecialist approach

Evidence-based recommendations for balancing cancer control with quality of life

Study shows no negative impact for individuals with better contralateral ear performance

HNS device offers new solution for those struggling with CPAP

Patient with cerebral palsy undergoes life-saving tumor resection

Specialists are increasingly relying on otolaryngologists for evaluation and treatment of the complex condition

Detailed surgical process uncovers extensive middle ear damage causing severe pain and pressure.